Understanding ADHD Stimulant Abuse: What You Need to Know
ADHD stimulant abuse refers to using prescription medications for Attention-Deficit/Hyperactivity Disorder in ways other than prescribed—taking higher doses, using someone else’s medication, or taking the medication solely to get high or improve performance. Here’s what you need to know:
Key Facts About ADHD Stimulant Abuse:
- Prevalence: More than 1 in 10 youth (10.4%) report past-year prescription stimulant misuse
- Diversion: 16-29% of students with prescriptions have been asked to give, sell, or trade their medication
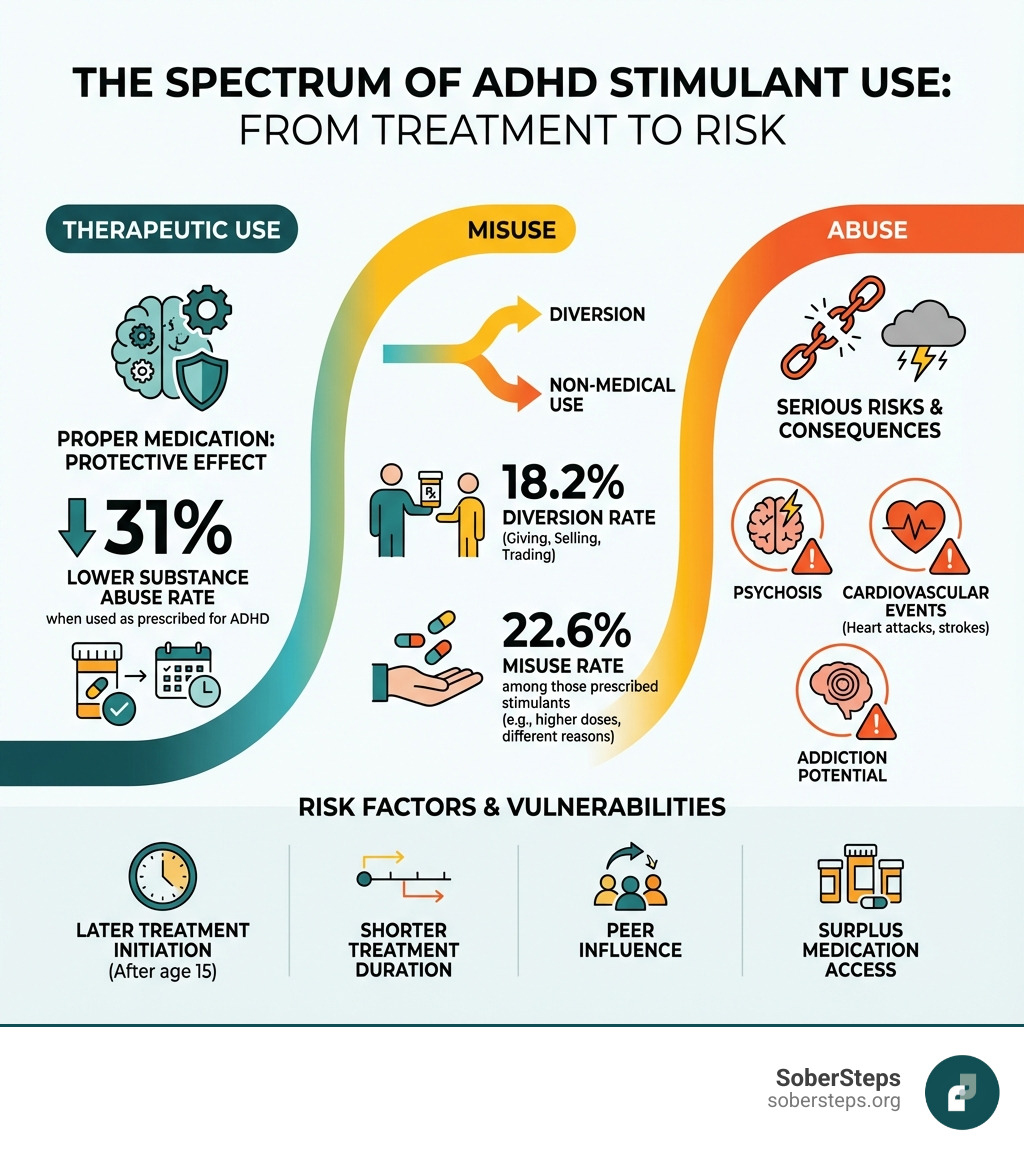
- Risk Factors: Later treatment initiation (after age 15), shorter treatment duration, peer influence, and surplus medication increase abuse risk
- Health Dangers: Large doses can cause psychosis, seizures, heart attacks, and strokes
- The Paradox: When used as prescribed for ADHD, stimulants reduce substance abuse risk by 31%
Children and adolescents with ADHD face a challenging reality. They’re at increased risk for developing substance use disorders—yet the medications proven most effective for treating their condition are stimulants, which themselves carry abuse potential. This creates confusion and fear for families trying to make the right treatment decisions.
The truth is more nuanced than many realize. Research shows that prescription stimulants like methylphenidate (Ritalin, Concerta) and amphetamines (Adderall) are highly effective treatments for ADHD when used properly. Studies indicate they help about 65-75% of children and adolescents with ADHD feel more focused and improve their functioning. The problem arises when these medications are misused—either by the person prescribed them or by others who obtain them illegally.
Understanding the difference between therapeutic use, misuse, and abuse is critical:
- Therapeutic Use: Taking your prescribed stimulant medication exactly as directed by your doctor for ADHD treatment
- Misuse: Taking your own medication differently than prescribed (higher doses, more frequently, or for reasons other than ADHD symptoms)
- Abuse: Using stimulants without a prescription, taking someone else’s medication, or using it solely to get high or improve performance
- Diversion: Giving, selling, or trading your prescribed medication to others
At Sober Steps, we’ve supported countless individuals and families navigating the complexities of ADHD stimulant abuse and addiction recovery. Our mission is to provide clear, evidence-based information that helps you make informed decisions about treatment and recognize when help is needed.
The statistics are sobering. An estimated 8.2% of youth have received stimulant therapy for ADHD at some point, yet 10.4% of all youth report past-year prescription stimulant misuse—meaning many people using these drugs don’t have ADHD at all. On college campuses, rates climb even higher, with 5-35% of students reporting nonprescription stimulant use. Students call them “study drugs” or “smart pills,” believing they’ll boost academic performance, when research shows they often don’t help and can cause serious harm.
The good news? When prescribed appropriately and monitored carefully, stimulant treatment for ADHD is not only safe but protective. Youth who start treatment early (before age 10) and continue it longer have 2-4 times lower rates of substance abuse compared to those who delay treatment or stop early. The medication itself, when used correctly, reduces impulsivity and promotes adaptive behaviors that decrease substance use risk.
The concerning news? Misuse carries real dangers—from cardiovascular events and psychosis to addiction and overdose. With stimulant-related overdose deaths increasing 10-fold in the past decade, understanding the risks has never been more important.
If you or a loved one is struggling with stimulant misuse, our confidential 24/7 helpline can connect you with treatment options.
This guide will help you understand the complex relationship between ADHD, stimulant treatment, and substance abuse. You’ll learn who’s at risk, why misuse happens, what the dangers are, and how to prevent problems while still getting effective ADHD treatment. Whether you’re a patient, parent, or clinician, you’ll find practical, science-backed information to make informed decisions.
The Protective Effect vs. The Risk: Does ADHD Treatment Cause Substance Abuse?
One of the most persistent concerns surrounding ADHD stimulant medication is whether it increases the risk of substance abuse. It’s a valid question, given that stimulants are controlled substances with abuse potential. However, a growing body of research suggests a surprising and reassuring answer: when used as prescribed, stimulant treatment for ADHD can actually reduce the risk of substance use disorders (SUDs).
To understand this, we first need to acknowledge that individuals with untreated ADHD are inherently at a higher risk for SUDs. Adults with ADHD are 2-3 times more likely to develop a SUD than their peers without ADHD. This increased vulnerability stems from several factors, including:
- Impulsivity and sensation-seeking: Core ADHD symptoms can lead to poor executive functioning and a lack of self-restraint, making individuals more prone to experimenting with substances.
- Hypodopaminergic state: ADHD and SUDs often share an underlying neurobiological basis, particularly a “hypodopaminergic state” where the brain’s reward system may be impaired. This can lead individuals to seek external stimulation to achieve normal reward responses.
- Self-medication: Some individuals with untreated ADHD may turn to substances to alleviate their symptoms, such as using stimulants to focus or depressants to calm an overactive mind.
- Comorbidity: Co-occurring conditions like conduct disorder further amplify the risk.
Effective pharmacological treatment for ADHD can mitigate these risks. By managing core ADHD symptoms like impulsivity and inattention, stimulant medications help individuals develop better coping mechanisms and adaptive behaviors. This, in turn, can reduce their vulnerability to substance use.
Studies, including a significant one using Swedish national registers, found that stimulant ADHD medication was not associated with an increased rate of substance abuse. In fact, among those prescribed medication, the rate of substance abuse was 31% lower after controlling for various factors. This protective effect was even stronger in children (15 years or younger). Another study focusing on adolescents found that prescribed stimulant therapy for ADHD was not associated with an increased risk of later cocaine and methamphetamine use during young adulthood, suggesting a protective effect against illicit stimulant use.
The clinical implication here is profound: delaying appropriate ADHD treatment may carry additional risks, including increased vulnerability to illicit substance use and prescription stimulant misuse later in life. We understand the concerns, but the evidence points towards a significant protective benefit of proper, monitored treatment.
If you or someone you know is struggling with co-occurring ADHD and a substance use disorder, it’s crucial to seek specialized care. Find help for co-occurring disorders through our dedicated resources. Understanding that ADHD itself is a risk factor for addiction means treating both conditions simultaneously is often the most effective path to recovery. Explore our pages on Dual Diagnosis ADHD and Dual Diagnosis to learn more about integrated treatment approaches.
How Treatment Timing and Duration Matter
The timing of when stimulant therapy for ADHD begins and how long it continues plays a critical role in shaping the risk of later substance use. This isn’t just about whether someone takes medication, but when and for how long.
Research, particularly a recent study involving Dr. Timothy Wilens, Chief of the Division of Child and Adolescent Psychiatry at Mass General Hospital, analyzed data to examine whether the age of initiation and duration of treatment impacted later risks. The findings were compelling:
- Later Initiation, Higher Risk: Youth who began stimulant therapy for ADHD after 15 years of age and reported a shorter duration of treatment were 2 to 4 times more likely to report stimulant prescription misuse, cocaine use, or methamphetamine use compared to those who started treatment before age 10 and continued it for a longer period.
- Earlier Start, Longer Protection: Conversely, earlier initiation of stimulant therapy and a longer duration of treatment for ADHD were consistently associated with a lower risk for prescription stimulant misuse and cocaine use in late adolescence. The Swedish study further supports this, showing that the longer an individual remains on stimulant medication, the lower their rate of substance abuse—a 13% decrease per year on medication.
These findings highlight a “sensitive developmental period” for ADHD treatment initiation. Delaying treatment may leave individuals vulnerable during critical years when substance use patterns often emerge. Adolescents with undiagnosed ADHD, for instance, have substance abuse rates three to four times greater than those treated with stimulants, suggesting they might be attempting to self-medicate their symptoms.
For prescribers, these insights reinforce the importance of prompt evaluation for ADHD and underscore the potential risks associated with delaying stimulant treatment. It’s a delicate balance, but the evidence strongly suggests that appropriate and sustained treatment can be a protective factor.
Learn more about the scientific research on ADHD medication and substance abuse risk and consider the expert analysis by Timothy Wilens, MD, on the age of initiation and duration of stimulant therapy.
If you’re concerned about substance abuse, especially in the context of ADHD, explore effective interventions. Our Substance Abuse Treatment and Addiction resources can guide you to appropriate care.
Understanding the Scope of ADHD Stimulant Abuse
While prescribed stimulant therapy can be protective, the misuse and diversion of these medications remain a significant public health concern, particularly among young adults.
Prevalence of Misuse and Diversion:
- Overall Youth Misuse: More than one in ten (10.4%) of all youth in the U.S. report past-year prescription stimulant misuse, many without an ADHD diagnosis.
- Misuse Among Prescribed Individuals: Even among individuals prescribed stimulants for ADHD, the prevalence of past-year misuse is substantial, averaging 22.6%. This means some patients are taking their medication in ways not intended by their doctor, such as taking higher doses or using it for non-ADHD related reasons.
- Diversion Rates: The diversion of prescribed stimulants—giving, selling, or trading medication to others—is also prevalent. A meta-analysis found an average past-year diversion rate of 18.2%, and a lifetime diversion rate of 17.9% among those prescribed stimulants. This often starts earlier than many realize; one study found 10% of adolescents diverted their medication in the past year.
- College Campuses: This issue is particularly acute in college settings, where non-prescribed stimulant use ranges from 5% to 35%. Often referred to as “study drugs” or “smart pills,” these medications are frequently misused during exam periods. Roughly a third of college students with ADHD report selling or giving away their medication at least once. This problem is exacerbated by peer influence, as students with prescriptions are often pressured to share their medication. Lifetime rates of being asked to divert medication can be as high as 16-29% for students with prescriptions.

We at Sober Steps understand the intense pressures students face, but the perceived benefits of these “study drugs” are often misleading and carry serious risks. If you or a loved one is struggling with the pressures that lead to stimulant misuse, help is available. Explore addiction success stories and know that you can Get Help Now.
Who Is at Risk and Why?
Several factors increase an individual’s risk for stimulant medication misuse and diversion, even among those legitimately prescribed the drugs for ADHD:
- Type of Stimulant: Being prescribed an amphetamine-based stimulant (like Adderall) may carry a higher risk of misuse compared to methylphenidate (like Ritalin).
- Comorbid Conditions: Individuals reporting co-occurring depressive and anxiety symptoms are at an liftd risk for misuse.
- Beliefs About Risk: Those who misuse stimulants are often less concerned with the ethics of misuse and are more likely to believe that non-medical use carries little to no risk. They may also perceive misuse as socially acceptable.
- Peer Influence and Exposure: Exposure to peers who are misusing stimulant medication is a significant risk factor for both misuse and diversion. If friends are using or asking for stimulants, it increases the likelihood of an individual engaging in these behaviors.
- Surplus Medication: Having extra medication available beyond what is needed for daily therapeutic use increases the risk of diversion. This can happen if dosages are adjusted or if patients don’t take their medication consistently.
- History of Substance Use: A history of substance use (alcohol, marijuana, ecstasy, painkillers) is strongly associated with a higher risk of diversion.
- Impulsivity and Lack of Self-Restraint: Core ADHD symptoms, particularly impulsivity, can make individuals more vulnerable to making poor decisions regarding their medication.
- Undiagnosed ADHD: Adolescents with undiagnosed ADHD have a significantly higher rate of substance abuse, suggesting that some misuse might be an attempt to self-medicate their symptoms. Non-prescription holders who misuse stimulants are also more likely to self-diagnose themselves with ADHD.
- Male Gender: Some studies have indicated that male gender is significantly associated with an increased risk of diversion.
These risk factors highlight the complex interplay of individual vulnerabilities, environmental influences, and access to medication. It’s crucial for both patients and healthcare providers to be aware of these indicators. If you’re concerned about risk factors for yourself or a loved one, please call our 24/7 helpline for a confidential risk assessment. Our team can provide Confidential Mental Health Support and connect you with Behavioral Health Support custom to your needs.
Motivations Behind ADHD Stimulant Abuse
The reasons people misuse or abuse ADHD stimulants are varied and often depend on whether they have an ADHD diagnosis or not. Understanding these motivations is key to prevention and intervention.
Motivations for Misuse (Individuals with and without ADHD):
- Academic Improvement (“Study Drugs”): This is by far the most common motivation, especially among college students. Users believe stimulants will:
- Improve concentration (cited by 65% of students).
- Help with studying (cited by 60% of students).
- Increase alertness or stay awake for longer periods (cited by 23.4% of illicit users).
- The perception is that these are “smart pills” that boost cognitive performance. However, research indicates that while stimulants may aid rote learning or long-term retention for simple tasks, they don’t significantly improve complex cognitive functions or improve academic performance in healthy individuals. In fact, higher doses can actually decrease performance and illicit use has a negative relationship with academic achievement.
- Recreational Use: Some individuals use stimulants to “get high” or seek euphoria (cited by 6.3% of illicit users). They may also use them to heighten the effects of alcohol or other drugs.
- Weight Loss/Appetite Control: Stimulants can suppress appetite, leading some to misuse them for cosmetic weight loss (cited by 3.6% of illicit users) or appetite control (cited by 4.2% of illicit users).
- Athletic Performance: Athletes might misuse stimulants to improve physical performance or maintain focus during sports. The World Anti-Doping Agency (WADA) bans most stimulants, and athletes often require therapeutic use exemptions (TUEs) for legitimate ADHD treatment.
- Self-Medication: This is particularly relevant for individuals with undiagnosed ADHD. They may use stimulants obtained illicitly to manage their own perceived symptoms of inattention, lack of focus, or low energy. Non-prescription holders who misuse stimulants are more likely to self-diagnose themselves with ADHD.
- Other Motives: These can include increasing energy, enhancing exercise, counteracting the effects of other drugs, or simply experimenting.
Differences in Reasons for Misuse:
While some motivations overlap, there are nuances. Individuals with an ADHD diagnosis who misuse their own medication might be seeking a stronger effect than prescribed, or trying to manage breakthrough symptoms. Those without a diagnosis are more likely driven by the “cognitive improvement” myth or recreational purposes.
| Motivation Category | Individuals with ADHD (Misusing their own Rx) | Individuals without ADHD (Illicit Users) |
|---|---|---|
| Academic/Work Performance | Often to maintain focus, catch up, or complete tasks beyond prescribed dosage. | Primarily driven by the “smart pill” myth; belief in improved concentration/alertness. |
| Recreational Use | Less common as primary motivation, but can occur, especially with higher doses. | Common motivation for seeking euphoria or enhancing other drug effects. |
| Self-Medication | May take higher doses to cope with severe symptoms or stress. | Often attempt to self-treat undiagnosed ADHD symptoms or general fatigue. |
| Weight Loss/Athletics | Possible, but not the primary driver for therapeutic users. | More common as a non-therapeutic use case. |
| Perception of Risk | May underestimate risks but often understand the drug’s purpose. | Often have less concern about health risks, perceive misuse as socially acceptable. |
We offer Online Mental Health and Mental Health Clinic services to help individuals address underlying mental health concerns that might contribute to self-medication or misuse.
The Dangers of Misusing Stimulant Medications
The allure of improved focus or a quick energy boost can be tempting, but misusing ADHD stimulant medications carries significant and potentially life-threatening health risks. These are powerful drugs, and when taken outside of a doctor’s guidance, their effects can be devastating.
1. Addiction Potential:
Perhaps the most immediate danger is the risk of addiction. If stimulants are taken at doses or by methods other than those prescribed by a healthcare provider (e.g., crushing and snorting, or injecting), they can be highly addictive. This is due to their pharmacological similarity to illicit drugs like cocaine, affecting the brain’s reward pathways. The DEA classifies stimulants as Class II controlled substances precisely because of their high potential for abuse and dependence.
2. Cardiovascular Risks:
Stimulants directly impact the cardiovascular system. Misuse, especially at high doses, can:
- Drive up blood pressure and heart rate: This puts immense strain on the heart.
- Increase body temperature.
- Cause a stroke: At high doses, the risk of stroke significantly increases.
- Lead to serious cardiac events: These include myocardial infarction (heart attack), cardiomyopathy (weakening of the heart muscle), and even sudden death. These risks are not theoretical; cases of myocardial infarction and inverted-Takotsubo cardiomyopathy have been linked to Adderall overdose. While prescribed use for ADHD does not appear to increase the risk for abnormal blood pressure elevations over the long term, misuse bypasses these safety parameters.
3. Psychological Consequences:
Repeated misuse can have severe psychological impacts, including:
- Psychosis: Large doses of stimulants can induce psychotic episodes, characterized by hallucinations, delusions, and disorganized thinking.
- Extreme anger and paranoia: Users may experience intense irritability, aggression, and become overly suspicious and distrustful.
- Anxiety and confusion: Unexplained anxiety, excitability, and confusion are common warning signs of misuse.
- Depression and violence: These can also emerge as symptoms of stimulant abuse.
4. Other Health Problems:
Misuse often leads to other health issues due to lack of sleep, poor nutrition, and the body being pushed beyond its limits. Non-oral routes of administration, such as snorting or injecting, carry additional severe risks like lung damage, infections, and fatal pulmonary hypertension.
For a comprehensive overview of these dangers, we encourage you to review a systematic review of stimulant misuse. Understanding these risks is the first step in preventing harm. If you or a loved one is struggling with stimulant misuse, please know that our Addiction/Drugs and Stimulant Addiction resources are here to help you find a path to recovery.
Long-Term Consequences of Abuse
The immediate dangers of stimulant misuse can be severe, but the long-term consequences can be equally devastating, impacting physical health, mental well-being, and overall quality of life.
1. Dependence and Withdrawal:
Chronic misuse leads to physical and psychological dependence. The body adapts to the presence of the stimulant, requiring higher doses to achieve the same effects (tolerance). If use is stopped abruptly, painful withdrawal symptoms can occur, including:
- Severe depression: This can be profound and lead to suicidal ideation.
- Overwhelming fatigue: Users often experience extreme exhaustion and lack of energy.
- Sleep problems: Insomnia or hypersomnia (excessive sleeping) can persist for weeks.
- Intense cravings: The urge to use more stimulants to alleviate withdrawal symptoms is powerful.
2. Lasting Brain Changes:
While more research is needed on the long-term effects of chronic misuse, we know that prolonged substance abuse can lead to changes in brain structure and function, particularly in areas related to reward, motivation, and impulse control. This can make it even harder to stop using and maintain recovery.
3. Exacerbation of Mental Health Issues:
For individuals with ADHD, chronic stimulant abuse can worsen underlying symptoms and lead to new mental health challenges, trapping them in a cycle of misuse and declining well-being. The paranoia and anger experienced during acute misuse can become more entrenched personality traits over time.
4. Legal and Social Ramifications:
Beyond health, long-term abuse can lead to legal issues related to illegal possession or diversion, academic failure, job loss, financial problems, and strained relationships. For medical professionals, stimulant misuse can result in severe professional consequences, including disciplinary action, loss of licensure, and an end to their career.
There are currently no FDA-approved medications specifically for addiction to prescription stimulant medication; treatment primarily relies on behavioral therapies. If you or a loved one is facing these challenges, seek professional help. Learn about stimulant addiction treatment and explore our resources on Drug Treatment Options and Drug Rehab to find effective support.
Prevention and Safety: A Guide for Patients, Parents, and Clinicians
Mitigating the risks of ADHD stimulant misuse and diversion requires a multi-faceted approach involving patients, their families, and healthcare providers. Our goal at Sober Steps is to empower everyone involved with the knowledge and tools to ensure safe and effective treatment.
For Patients:
- Strict Adherence to Prescriptions: Always take your stimulant medication exactly as prescribed by your doctor. Do not alter the dose, frequency, or method of administration without consulting your clinician.
- Understand the Risks: Be fully aware of the serious health risks associated with misuse, including addiction, cardiovascular problems, and psychological issues.
- Do Not Share or Sell Medication: It is illegal and extremely dangerous to give, sell, or trade your prescribed medication to anyone else. This is called diversion and carries severe consequences for both the giver and the recipient.
- Open Communication: Maintain an honest and open dialogue with your healthcare provider about how your medication is affecting you, any concerns about side effects, or any cravings or thoughts of misuse.
For Parents:
- Education and Open Dialogue: Discuss the importance of using medication only as prescribed and the dangers of sharing with your child. Foster an environment where your child feels comfortable discussing their studies, performance, and any pressures they may face.
- Safe Medication Storage: Keep all stimulant medications in a secure, locked location, out of reach and sight of children, adolescents, and visitors. Regularly check the medication count to ensure none is missing.
- Monitor for Warning Signs: Be vigilant for signs of stimulant abuse in your child, which may include:
- Going long periods without sleeping or eating.
- Unexplained weight loss.
- Excessive activity or restlessness.
- Extreme talkativeness or an overly high mood.
- Increased grouchiness, nervousness, or irritability.
- Pupils that are larger than usual.
- Unexplained anxiety, confusion, or even violent outbursts.
- Lead by Example: Model responsible behavior regarding medication use and avoiding substance abuse.
- Seek Support: If you observe warning signs, approach your child in a supportive, caring manner. Consider seeking professional guidance to address your concerns.
For Clinicians:
- Thorough Diagnosis and Risk Assessment: Use standardized screening tools and comprehensive neuropsychiatric evaluations for accurate ADHD diagnosis. Before prescribing, conduct a thorough risk assessment for substance misuse and diversion, considering factors like a patient’s history of substance use, peer stimulant misuse, and beliefs about misuse risks.
- Patient Education: Educate patients and their families about the risks of abuse and dependence, the importance of adherence, and the dangers of diversion (especially intravenous administration).
- Prescription Practices:
- Consider prescribing extended-release formulations over immediate-release, as they generally have lower abuse potential.
- Prioritize non-stimulant medications (e.g., atomoxetine, bupropion) for patients at high risk of substance abuse or when stimulants are ineffective or contraindicated.
- Limit the number of pills per dispensation (e.g., 30-day supply) and monitor closely.
- Ongoing Monitoring:
- Carefully monitor patient response to prescribed stimulants using rating scales.
- Assess requests for dosage increases or early refills to rule out misuse or diversion.
- Inquire about leftover medication or “stockpiles” to assess adherence.
- Be “on the alert” for signs of misuse, particularly during stressful academic periods.
- Consider toxicology testing when clinically indicated.
- Collaboration and Communication: Foster open communication with patients. Implement brief interventions at clinical encounters, potentially using tools like the FOCUS checklist (F for family/friends, O for others, C for care, U for use, S for storage) to guide discussions on misuse and diversion.
Creating a Safe Treatment Environment
A safe and effective treatment environment for ADHD, particularly when stimulants are involved, relies on a foundation of trust, education, and collaboration.
- Open Communication Channels: Encourage an open and honest dialogue between patients, parents, and clinicians. Patients should feel comfortable discussing any challenges or concerns without fear of judgment. Parents should also communicate openly with their children about medication use and potential pressures.
- Strong Doctor-Patient Relationship: A solid relationship with a healthcare provider who understands the nuances of ADHD and substance use risk is paramount. This allows for personalized care, continuous monitoring, and adjustments as needed.
- Regular Follow-Up Appointments: Consistent check-ins are crucial to monitor medication effectiveness, side effects, and adherence, as well as to reassess any risks for misuse or diversion.
- School and Family Collaboration: For younger patients, collaboration between parents, clinicians, and school personnel can create a supportive network, ensuring consistent management and early identification of issues.
- Non-Stimulant Medication Options: For individuals where stimulants are not suitable, or for those at higher risk of substance abuse, non-stimulant medications provide valuable alternatives. These medications, such as atomoxetine, guanfacine, or clonidine, can effectively manage ADHD symptoms without the same abuse potential. Behavioral therapies, including Cognitive Behavioral Therapy (CBT), coaching, and biofeedback, are also highly effective non-pharmacological strategies that can be used alone or in conjunction with medication.
We believe in empowering individuals with the best possible care. Whether you’re considering medication, exploring therapy options, or seeking support for a stimulant use disorder, we can help. Explore safe and effective treatment options today including Individual Therapy Addiction, Therapy, and Cognitive Behavioral Therapy. Our resources on Levels of Care and Treatment can guide you further.
Conclusion: Balancing Treatment and Responsibility
The journey through ADHD treatment, especially involving stimulant medications, is a complex one, fraught with both significant benefits and potential risks. We’ve seen that when prescribed and monitored correctly, stimulant therapy for ADHD is not only effective in managing symptoms but can also act as a protective factor against the development of substance use disorders. This challenges the common misconception that ADHD medications inherently lead to addiction.
However, the reality of ADHD stimulant abuse and diversion remains a serious public health concern, particularly among adolescents and young adults. Misuse, often driven by a misguided belief in cognitive improvement or by attempts to self-medicate, carries severe health risks, including cardiovascular events, psychosis, and addiction.
Balancing the therapeutic benefits with the risks of misuse requires vigilance, education, and open communication from all involved parties—patients, parents, and clinicians. By understanding the nuances of how treatment timing and duration impact outcomes, recognizing risk factors and motivations for misuse, and implementing robust prevention strategies, we can ensure that individuals with ADHD receive the care they need while minimizing potential harm.
At Sober Steps, we are committed to providing clear, evidence-based information and connecting individuals and families with the support they deserve. If you or a loved one is navigating the complexities of ADHD and potential substance use concerns, remember you don’t have to do it alone. Contact our confidential helpline for recovery options and support. Our team can also help you Verify Insurance and understand your Insurance coverage for treatment.



