Understanding the Complexity of Co-Occurring Disorders
Co-occurring disorders treatment addresses the complex challenge of managing both a substance use disorder and a mental health condition simultaneously. When you’re facing both addiction and mental illness, specialized integrated care is essential for effective recovery.
Quick Answer: What You Need to Know About Co-Occurring Disorders Treatment
- What it is: Simultaneous treatment for both substance use disorders and mental health conditions by the same care team
- Why it matters: About 9.2 million adults in the U.S. have co-occurring disorders, but over 50% never receive treatment
- The gold standard: Integrated treatment (treating both conditions together) produces better outcomes than treating them separately
- Key components: Therapy (CBT, DBT), medication when needed, peer support, and personalized care plans
- Treatment settings: Options range from medical detox and inpatient care to outpatient programs
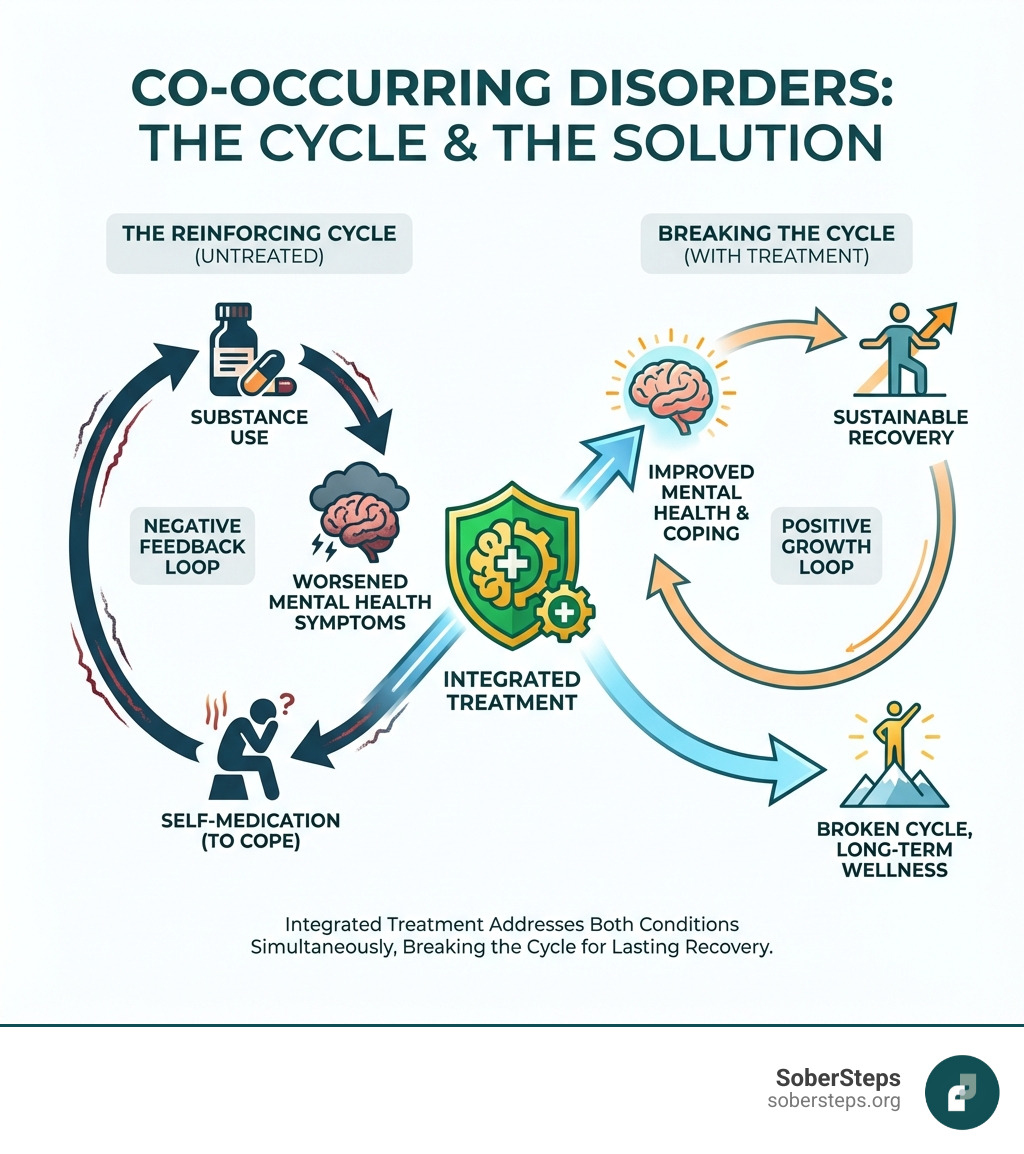
The reality is sobering: if you’re struggling with addiction, there’s nearly a 50% chance you’re also dealing with a mental health condition like depression, anxiety, or PTSD. These conditions don’t just exist side-by-side—they influence and worsen each other in a cycle that can feel impossible to break.
In the past, mental health and addiction were treated separately. This fragmented approach often failed, as it didn’t address the complex interplay between the conditions.
Today, we know better. Integrated treatment—where the same team addresses both your mental health and substance use at the same time—is now recognized as the standard of care. It’s not just more convenient; it’s significantly more effective.
At Sober Steps, we specialize in connecting individuals with comprehensive co-occurring disorders treatment that addresses the full scope of addiction and mental health challenges. Our confidential platform has helped thousands find the specialized, integrated care they need to reclaim their lives. If you’re ready to explore treatment options that address all of your needs, call us at (844) 491-5566 to speak with a compassionate specialist.
Understanding Co-Occurring Disorders
Co-occurring disorders, or dual diagnosis, means having both a substance use disorder (SUD) and a mental health condition. These conditions are deeply interconnected, influencing and often exacerbating each other. Treating them in isolation is often ineffective.
The connection is complex and bidirectional. Sometimes, a mental health condition appears first, leading a person to use substances to cope with symptoms (the “self-medication hypothesis”). For example, someone with anxiety might use alcohol to calm their nerves. While this may offer temporary relief, it ultimately worsens the underlying mental health issue and can lead to addiction.
Conversely, chronic substance abuse can trigger or worsen mental health conditions. Drugs and alcohol alter brain chemistry, which can manifest as depression, anxiety, or psychosis. This creates a vicious cycle: substance use worsens mental health, which in turn fuels more substance use.
Prevalence and Statistics
The scope of co-occurring disorders is vast. According to SAMHSA’s 2021 National Survey on Drug Use and Health, 9.2 million U.S. adults have a co-occurring disorder, making it a major public health concern.
Consider these key statistics:
- Over a third of adults with SUDs also have a mental illness.
- Nearly 20% of those with a mental health condition also have an SUD.
- Shockingly, over 50% of people with co-occurring disorders receive no treatment for either condition, often due to cost.
These numbers highlight a critical treatment gap. In 2019, only 7.8% of adults with co-occurring disorders received care for both conditions, underscoring the need for more accessible, integrated treatment.
Common Co-Occurring Conditions
While any mental health condition can co-occur with an SUD, some pairings are more common. Understanding these helps in tailoring effective co-occurring disorders treatment.
- Anxiety Disorders and SUD: People with anxiety may use substances like alcohol to self-medicate intense fear and worry.
- Mood Disorders (Depression, Bipolar Disorder) and SUD: Depression is a very common co-occurrence, with individuals using substances to numb sadness. Those with bipolar disorder may use substances during mood episodes.
- Post-Traumatic Stress Disorder (PTSD) and SUD: Trauma survivors are up to four times more likely to have an SUD, often using substances to escape painful memories.
- Personality Disorders and SUD: Conditions like borderline personality disorder can contribute to impulsive behaviors, including substance abuse. The prevalence of personality disorders is significantly higher in those treated for addiction compared to the general population.
- Schizophrenia and SUD: About 25% of people with a severe mental illness like schizophrenia also have an SUD, sometimes to cope with symptoms like hallucinations.
- Attention-Deficit/Hyperactivity Disorder (ADHD) and SUD: Individuals with ADHD may be more prone to impulsive substance use or may use substances to self-medicate symptoms like restlessness.
Causes and Risk Factors
Co-occurring disorders rarely have a single cause. They result from a complex interplay of factors:
- Genetic Predisposition: A family history of either mental illness or addiction can increase susceptibility.
- Environmental Stressors: Chronic stress, poverty, and lack of social support are contributing factors.
- Trauma and Adverse Childhood Experiences (ACEs): Trauma is a significant risk factor, impacting brain development and emotional regulation, making substance use a more likely coping mechanism.
- Brain Chemistry Changes: Both mental illness and substance use involve alterations in brain function related to pleasure, stress, and impulse control.
- Overlapping Risk Factors: Many risk factors, such as impulsivity or poor coping skills, are common to both mental illness and SUDs.
Signs, Symptoms, and Professional Assessment
Recognizing the signs of co-occurring disorders can be challenging because symptoms often overlap. However, being aware of common indicators is the first step toward seeking help.
Look for changes in behavior, mood, and physical health, such as:
- Significant changes in sleep or appetite.
- Extreme mood swings, irritability, or persistent sadness and anxiety.
- Withdrawal from social activities and hobbies.
- Engaging in risky or impulsive behaviors.
- Difficulty concentrating or making decisions.
- Neglecting responsibilities at work, school, or home.
- Experiencing withdrawal symptoms or an inability to control substance use.

The Challenge of Diagnosis
Diagnosing co-occurring disorders is challenging due to symptom overlap. For instance, fatigue from depression can mimic chronic drug use, while anxiety can mirror stimulant abuse. Substances can also mask or mimic mental illness symptoms; alcohol can intensify depression, while stimulants can induce paranoia. This makes it hard to tell if symptoms stem from a mental health condition, substance use, or both.
For an accurate diagnosis, a period of abstinence is often crucial. This allows professionals to assess mental health symptoms without the confounding effects of intoxication or withdrawal. The “No Wrong Door” policy is also vital, advocating for screening for both conditions whenever a person enters the healthcare system, regardless of their initial complaint.
The Assessment and Diagnostic Process
A comprehensive assessment is the foundation of effective co-occurring disorders treatment. It goes beyond symptoms to understand the individual’s history and the interplay between their conditions.
A typical assessment includes:
- Comprehensive Biopsychosocial Assessment: A thorough review of biological (genetics, medical history), psychological (trauma, coping skills), and social (family, employment) factors.
- Screening Tools: Standardized tools like the AUDIT for alcohol use, PHQ-9 for depression, and GAD-7 for anxiety help identify potential issues.
- Medical Evaluation: A physical exam and lab tests rule out other medical conditions and assess the physical impact of substance use.
- Psychiatric Evaluation: A mental health professional conducts a detailed interview to diagnose any mental health conditions based on established criteria (e.g., DSM-5), differentiating between substance-induced and independent disorders.
The Substance Abuse and Mental Health Services Administration (SAMHSA) provides extensive guidance on this process in its Treatment Improvement Protocols, such as “Substance Abuse Treatment for Persons With Co-Occurring Disorders.”
Integrated Co-Occurring Disorders Treatment: The Gold Standard
Integrated treatment is the gold standard for co-occurring disorders, where one clinical team treats both the SUD and mental health condition simultaneously. This is far more effective than older, separate treatment models.
In an integrated model, care is coordinated and seamless. The treatment team—which may include psychiatrists, therapists, and addiction specialists—works together on a unified plan. This ensures that interventions for one condition don’t undermine progress in the other. For example, an addiction specialist will be aware of any medications prescribed for depression and factor them into the substance use treatment plan.
Benefits of an Integrated Approach
By treating both conditions concurrently, integrated co-occurring disorders treatment leads to significantly better outcomes.
Benefits include:
- Improved psychiatric symptoms
- Reduced or discontinued substance use
- Increased housing stability
- Fewer arrests
- Higher quality of life
- Better treatment retention
- Decreased hospitalization
- Reduced medication interactions
Integrated treatment provides comprehensive care that supports all areas of a person’s life, fostering a more sustainable and fulfilling recovery.
Key Components of an Effective Program
An effective co-occurring disorders treatment program delivers integrated services with a specific philosophy and set of practices.
- Person-Centered Care: Treatment plans are customized to the individual’s unique needs and goals, with their active involvement.
- Trauma-Informed Approach: Care is delivered in a way that recognizes the impact of trauma, avoids re-traumatization, and supports healing.
- Recovery-Oriented Services: The focus is on supporting a meaningful life in the community, not just on symptom reduction. This includes building life skills and promoting long-term well-being.
- Evidence-Based Practices: Programs use therapeutic techniques that are scientifically proven to be effective for both substance use and mental health disorders.
- The Role of Therapy: As experts often discuss, therapy is vital in addiction treatment, helping individuals understand the root causes of their substance use and develop healthier coping mechanisms.
What an Integrated Treatment Plan Involves
An integrated treatment plan is a personalized, evolving roadmap to recovery developed by a multidisciplinary team of counselors, doctors, and therapists. It addresses all aspects of your health, outlining the levels of support needed throughout your journey.
| Treatment Setting | Description | Best Suited For |
|---|---|---|
| Inpatient/Residential | 24/7 supervised care in a facility. Provides a structured, safe environment away from triggers. | Severe SUDs, acute mental health crises, unstable home environments, or those needing intensive medical/psychiatric monitoring. |
| Partial Hospitalization Program (PHP) | Day treatment, usually 5-7 days a week, several hours a day. Patients return home or to a sober living facility at night. | Individuals needing structured care but with a stable home environment and less severe medical/psychiatric needs. |
| Intensive Outpatient Program (IOP) | More flexible than PHP, typically 3-5 days a week for a few hours. Allows for work or school commitments. | Those transitioning from higher levels of care, or with moderate symptoms and good support systems. |
| Standard Outpatient | Weekly or bi-weekly therapy sessions and support groups. Most flexible option. | Individuals with stable recovery, strong coping skills, and a solid support system, or for long-term aftercare. |
Therapeutic Interventions for Co-Occurring Disorders Treatment
Therapy is the backbone of co-occurring disorders treatment. Our integrated plans often incorporate a variety of evidence-based interventions:
- Cognitive Behavioral Therapy (CBT): Helps identify and change negative thought patterns and behaviors, teaching coping skills for triggers and stress.
- Dialectical Behavior Therapy (DBT): Focuses on emotional regulation, distress tolerance, interpersonal skills, and mindfulness. It’s highly effective for severe emotional dysregulation.
- Motivational Improvement Therapy (MET): Helps resolve ambivalence about treatment and strengthens motivation to change, especially in early recovery.
- Contingency Management: Uses positive reinforcement, such as tangible rewards, for desired behaviors like negative drug tests.
- Family Therapy: Involves loved ones to improve communication, repair relationships, and build a supportive home environment.
Medication and Support Systems
Medication often plays a crucial role in managing co-occurring disorders, especially when mental health symptoms are severe or when medication-assisted treatment (MAT) is needed.
- Medication-Assisted Treatment (MAT): For opioid and alcohol use disorders, MAT combines FDA-approved medications with counseling. It can reduce cravings and prevent relapse.
- Psychotropic Medications: Medications like antidepressants, mood stabilizers, or anti-anxiety drugs can help manage mental health symptoms, making it easier to engage in therapy. These are carefully monitored by a psychiatrist.
Beyond professional help, strong support systems are vital. Peer support offers invaluable emotional and social backing. At Sober Steps, we know supportive communities can help you stay sober and manage mental health. Connecting with others who share similar experiences reduces isolation and provides a sense of belonging.
Levels of Care for Co-Occurring Disorders Treatment
The path to recovery involves different levels of care to match your specific needs. For many, the first step is Medical Detoxification, a supervised process to safely manage withdrawal symptoms. From there, treatment can range from highly structured Inpatient/Residential Programs to more flexible Outpatient Programs (PHP, IOP, and Standard), as detailed in the table above. A quality program ensures smooth transitions between these levels as your needs evolve.
Navigating Treatment Access and Challenges
Despite the clear need for co-occurring disorders treatment, accessing it can be challenging. Many individuals face significant barriers on their path to recovery.
Common barriers to care include:
- Stigma: The societal judgment associated with mental illness and addiction can lead to shame and prevent people from seeking help.
- Financial Concerns: The cost of treatment can be a major deterrent, even with insurance.
- Lack of Available Programs: Finding specialized integrated care programs can be difficult, especially in rural areas.
- Logistical Issues: Transportation, childcare, and time off work can make it hard to commit to treatment.
Insurance Coverage for Dual Diagnosis
Fortunately, key legislation in the United States has expanded insurance coverage for co-occurring disorders treatment.
- Mental Health Parity and Addiction Equity Act (MHPAEA): This 2008 law requires most health plans to provide mental health and substance use benefits that are on par with medical/surgical benefits.
- Affordable Care Act (ACA): The ACA classified mental health and substance use disorder services as essential health benefits that most insurance plans must cover.
However, navigating insurance can still be complex. We recommend:
- Verifying Benefits: Contact your insurance provider to understand your specific plan’s coverage, including deductibles, co-pays, and pre-authorization rules.
- In-Network vs. Out-of-Network: In-network providers are typically cheaper. Understand your costs if you choose an out-of-network provider.
- Private Pay Options: Many centers offer private pay options, payment plans, or sliding scale fees for those without adequate insurance.
How to Find Quality Treatment
Finding the right co-occurring disorders treatment program is crucial. Be sure to research providers and ask key questions.
When looking for a provider, consider asking:
- Do you offer integrated treatment for both mental health and substance use disorders?
- What therapies and medications do you use?
- What are the credentials and licenses of your staff?
- Is your program accredited by bodies like The Joint Commission or CARF?
- What levels of care do you offer and how do patients transition between them?
- What is your approach to aftercare and relapse prevention?
A valuable resource is the Substance Abuse and Mental Health Services Administration (SAMHSA). Their behavioral health treatment service locator can be found here.
Finally, aftercare planning is essential. A good program will help you develop a robust plan that includes ongoing therapy, support groups, and strategies for maintaining long-term well-being.
Frequently Asked Questions about Co-Occurring Disorders
Is it better to treat the addiction or the mental health issue first?
The evidence-based standard is integrated treatment, which addresses both conditions simultaneously. Treating only one often leads to relapse because the issues are intertwined. For example, treating depression is difficult if substance use continues to affect brain chemistry.
Can substance abuse cause a mental illness?
Yes, substance abuse can cause or worsen mental illness. Drugs and alcohol can trigger an underlying predisposition or create new, substance-induced disorders like psychosis, anxiety, or depression. These effects on brain chemistry can persist even after stopping use.
What is the difference between ‘dual diagnosis’ and ‘co-occurring disorders’?
The terms ‘dual diagnosis’ and ‘co-occurring disorders’ are used interchangeably. They both refer to having a substance use disorder and a mental health disorder at the same time. ‘Co-occurring disorders’ is often preferred today as it can encompass more than two conditions, but both terms point to the need for integrated treatment.
Begin Your Confidential Path to Integrated Recovery
We’ve explored the complexities of co-occurring disorders, the profound impact they have on individuals, and the necessity of integrated co-occurring disorders treatment. We’ve seen that simultaneous care, custom to your unique needs, offers the most promising path to lasting recovery. It’s a journey that addresses both your mental health and substance use, recognizing their deep connection and ensuring no part of you is left behind.
At Sober Steps, we believe in the power of hope and the potential for every individual to achieve a fulfilling life free from the grip of addiction and mental illness. Our mission is to provide a confidential and anonymous platform where you can find the specialized help you deserve. We understand that taking the first step can be daunting, but you don’t have to steer this alone.
If you or a loved one is struggling with co-occurring disorders, confidential help is available. Our team can help you understand your options and find a path to recovery that addresses all of your needs. Call us at (844) 491-5566 to speak with a compassionate specialist today or learn more about specialized programs like female rehab centers. Your journey to custom recovery starts here.