
Beyond the Stigma: Understanding Modern Addiction Therapies
Discover how addiction is treated with modern therapies. SoberSteps guides you through detox, therapy, and long-term recovery.
UnitedHealth Group Insurance Coverage for Drug Rehab is available for most policyholders seeking treatment for substance use disorders. If you’re wondering whether your plan covers rehab, here’s what you need to know right now:
Quick Answer: Does UnitedHealth Group Cover Drug Rehab?
UnitedHealth Group is the largest health insurance company in the United States, serving over 150 million people through its UnitedHealthcare and Optum subsidiaries. Most plans—including individual marketplace plans, employer-sponsored coverage, Medicare Advantage, and many Medicaid plans—provide coverage for substance use disorder treatment at levels comparable to other medical care.
The challenge isn’t whether coverage exists—it’s understanding exactly what your specific plan covers. Different plan types have different rules about in-network providers, prior authorization requirements, and out-of-pocket costs. A Bronze marketplace plan works very differently than an employer-sponsored PPO, and those differences directly impact how much you’ll pay for treatment.
You don’t have to figure this out alone. At Sober Steps, we’ve helped thousands of individuals steer the complexities of UnitedHealth Group Insurance Coverage for Drug Rehab, verifying benefits and connecting people with appropriate treatment options. Our team understands how insurance works and can explain your coverage in plain language—call (844) 491-5566 anytime, day or night.
The Substance Use Helpline that UnitedHealthcare offers (1-855-780-5955) provides support and guidance, but you can also reach out directly to treatment providers like us who can verify your specific benefits and walk you through your options. Getting help starts with understanding what you’re entitled to—and what it will cost.
UnitedHealth Group (UHG) stands as a giant in the healthcare industry, serving over 152 million people across the United States. It’s the parent company to UnitedHealthcare, which is the actual insurance provider, and Optum, which focuses on health services, technology, and pharmacy benefits. This structure means that when we talk about UnitedHealth Group Insurance Coverage for Drug Rehab, we’re primarily referring to UnitedHealthcare plans, often integrated with Optum’s behavioral health services.
Understanding your UnitedHealthcare plan basics is the first step toward accessing addiction treatment. UnitedHealthcare offers a wide array of plans, including those bought on the Affordable Care Act (ACA) marketplace, employer-sponsored group benefit plans, Medicare Advantage plans for seniors and eligible individuals with disabilities, and Medicaid plans for low-income families and individuals in participating states. Each plan type comes with its own set of benefits, networks, and cost-sharing structures.
The good news is that legal mandates ensure robust coverage for substance use disorders. The Affordable Care Act (ACA), enacted in 2010, made mental health and substance abuse coverage an essential health benefit. This means that all ACA-compliant plans must cover services for these conditions. Furthermore, the Mental Health Parity and Addiction Equity Act (MHPAEA), passed in 2008, requires that coverage for mental health and substance use disorders be no more restrictive than coverage for medical and surgical benefits. In simple terms, your UnitedHealthcare plan can’t make it harder or more expensive to get treatment for addiction than it would for a broken leg or heart disease. You can learn more about this vital protection on the Healthcare.gov website regarding Mental Health and Substance Abuse Coverage.
However, coverage often hinges on what’s deemed “medical necessity.” This means a healthcare professional must determine that the treatment you’re seeking is appropriate and required for your condition. UnitedHealthcare, like all insurers, uses clinical criteria to make these determinations.
Finally, rest assured that your privacy is protected. Confidentiality and HIPAA (Health Insurance Portability and Accountability Act) regulations ensure that your personal health information, including details about your addiction treatment, remains private. When you call us at Sober Steps at (844) 491-5566, your conversations are completely confidential.
Yes, absolutely! UnitedHealthcare covers drug and alcohol rehab. Thanks to federal laws like the Affordable Care Act and the Mental Health Parity and Addiction Equity Act, most UnitedHealthcare plans are legally mandated to provide coverage for substance use disorder treatment. Addiction is recognized as a treatable disease, and insurance companies are required to treat it as such.
However, the extent of this coverage can vary significantly depending on your specific plan. For instance, a basic Bronze plan on the marketplace might have higher deductibles and coinsurance compared to a Gold plan or a comprehensive employer-sponsored PPO. We’ll dive deeper into plan types shortly, but for now, know that UnitedHealth Group Insurance Coverage for Drug Rehab is a reality for the vast majority of members.
A critical factor affecting your out-of-pocket costs will be whether the facility you choose is in-network or out-of-network. In-network providers have negotiated rates with UnitedHealthcare, typically resulting in lower costs for you. Out-of-network providers, while sometimes covered, often come with higher coinsurance or deductibles, and some plans may not cover them at all. It’s also worth noting that state-specific rules can sometimes add additional layers of coverage or requirements, so what’s covered in one state might have slightly different nuances in another.
To get a clear picture of your specific benefits, we encourage you to call (844) 491-5566 for a confidential benefits check. Our team can help you understand the specifics of your plan and how it applies to drug and alcohol rehab.
Yes, UnitedHealthcare generally provides coverage for co-occurring mental health disorders, often referred to as dual diagnosis treatment. It’s incredibly common for individuals struggling with substance use to also experience mental health conditions like depression, anxiety, or PTSD. In fact, research shows that treating both conditions simultaneously, through integrated care, leads to much better outcomes.
UnitedHealthcare explicitly categorizes substance misuse, behavioral health, and mental health treatment together. This means that their plans are designed to cover these services at the same level as other medical care, thanks to the MHPAEA. So, if you’re seeking treatment for addiction and also need support for depression, your UnitedHealthcare plan should cover both aspects of your integrated treatment plan. This ensures that you receive comprehensive care that addresses all facets of your well-being, not just one.

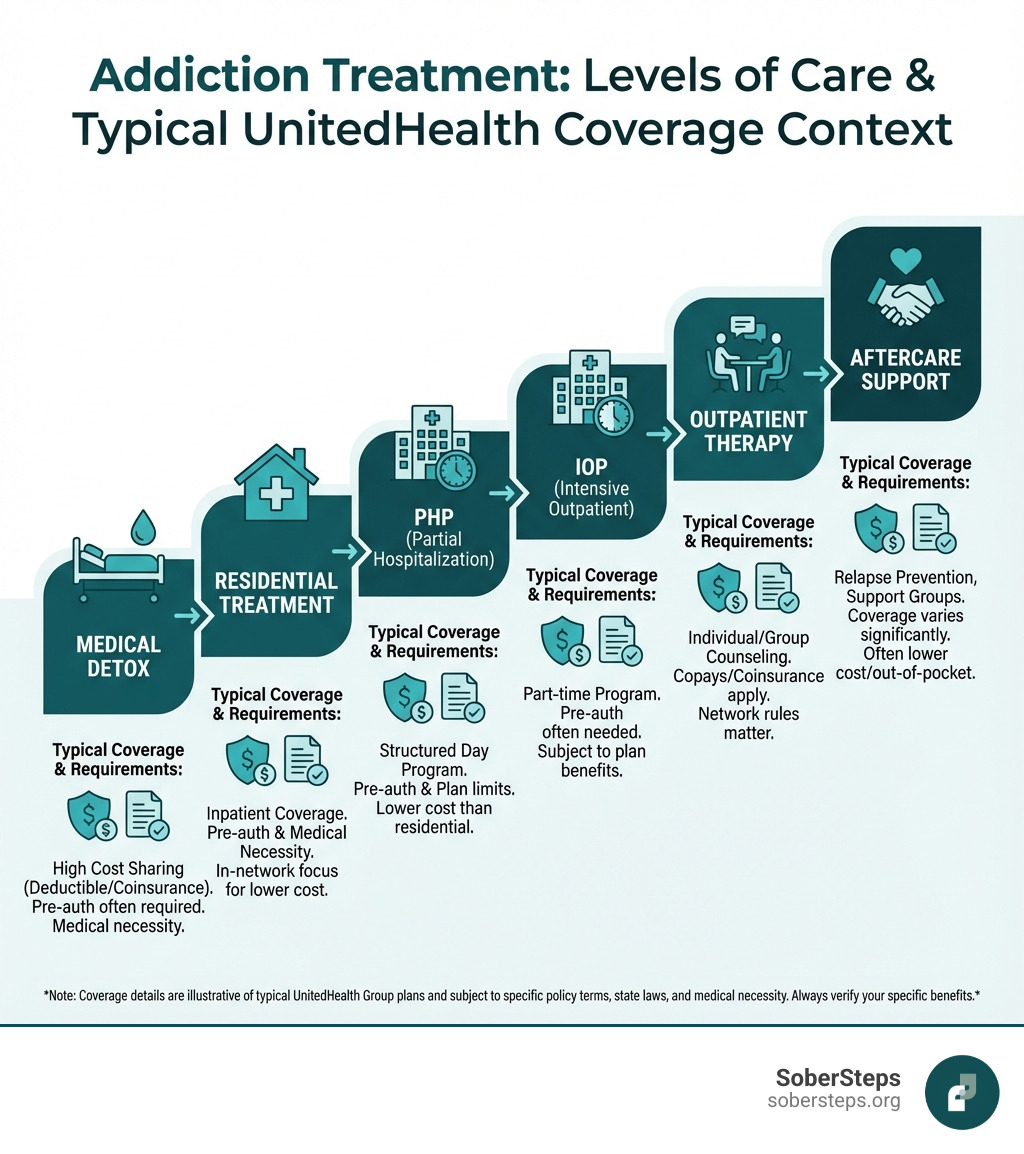
Addiction treatment is a journey, not a single event, and it involves a continuum of care with various levels and types of services. UnitedHealthcare plans are designed to cover a wide range of these services, particularly those considered evidence-based therapies, which have proven effectiveness. These often include individual and group therapy, family counseling, and other therapeutic modalities. The goal is always to provide an individualized treatment plan custom to your unique needs and circumstances.
To discuss your covered options and understand which types of treatment might be best for you, don’t hesitate to call our 24/7 helpline at (844) 491-5566.
Yes, most UnitedHealthcare plans cover medical detox. Medical detoxification, or withdrawal management, is often the critical first step in addiction recovery, especially for substances like alcohol and benzodiazepines, where withdrawal can be dangerous and even life-threatening without professional medical supervision. Opioid detox also benefits greatly from medical oversight to manage severe withdrawal symptoms.
UnitedHealthcare recognizes the medical necessity of detox services. Coverage typically extends to:
Detox can be provided in various settings, including dedicated inpatient detox facilities or as part of a broader residential treatment program. Outpatient detox may also be an option for individuals with less severe dependencies and strong support systems, allowing them to withdraw at home while attending daily medical appointments. The specific setting covered will depend on your medical needs and your plan’s benefits.
Yes, UnitedHealthcare plans typically cover both inpatient and outpatient treatment programs for substance use disorders. The level of care recommended will depend on the severity of the addiction, co-occurring mental health conditions, and individual circumstances.
Here’s a breakdown of common programs covered:
Yes, UnitedHealthcare generally covers Medication-Assisted Treatment (MAT) when it’s part of a comprehensive treatment plan. MAT combines FDA-approved medications with counseling and behavioral therapies, and it’s recognized as the most effective approach for treating opioid use disorder and alcohol use disorder.
Covered medications typically include:
MAT is not just about the medication; it’s about the combination of medication and therapeutic support. UnitedHealthcare’s coverage typically reflects this integrated approach, supporting the use of these medications when prescribed and monitored by qualified healthcare professionals as part of an overall recovery strategy.

Navigating insurance plans can feel like deciphering a secret code. Your UnitedHealthcare plan documents, especially the Summary of Benefits and Coverage (SBC), are your best friends here. These documents outline what your plan covers, your cost-sharing responsibilities, and any limitations. It’s also crucial to be aware of prior authorization requirements. Many addiction treatment services, especially inpatient programs, require pre-approval from UnitedHealthcare before you can begin treatment. Without it, your claim might be denied.
This process can be overwhelming, especially when you or a loved one is in crisis. Don’t wait, call (844) 491-5566 now for help. Our team can assist with understanding these documents and requirements.
UnitedHealthcare offers various plan types, and understanding them is key to predicting your coverage and costs for drug rehab:
In addition to these structural types, plans purchased on the ACA marketplace are categorized into “Metal” Tiers, which indicate how costs are shared between you and your insurer. You can read more about these categories on Healthcare.gov: The ‘metal’ categories explained.
For example, a Bronze plan might have a high deductible ($8,300) and 50% coinsurance for outpatient and inpatient addiction treatment. A Silver plan might have a $3,600 deductible, a $100 co-pay for office visits, and 40% coinsurance for inpatient/outpatient services. A Gold plan, with higher premiums, could offer a $2,000 deductible and 20% coinsurance for services. These examples highlight why understanding your specific plan is so crucial!
When using your UnitedHealthcare plan for drug rehab, you’ll encounter several terms that define your out-of-pocket costs:
Here’s a general idea of how these might look for marketplace plans, though specific numbers vary greatly:
| Plan Tier | Monthly Premium | Deductible (Example) | Coinsurance (Example) |
|---|---|---|---|
| Bronze | Lowest | Very High ($8,000+) | 40-50% |
| Silver | Moderate | Moderate ($3,000-$7,000) | 20-40% |
| Gold | Higher | Lower ($0-$3,000) | 10-20% |
These are examples. Your actual costs will depend on your specific UnitedHealthcare plan, the type of treatment, and whether the provider is in-network.
Finding a rehab facility that is in-network with UnitedHealthcare is crucial for managing your costs. Here are the best ways to do it:
The process of verifying your insurance coverage for drug rehab can seem daunting, but it’s a necessary step to ensure you understand your financial responsibilities and maximize your benefits. We aim to make this as smooth as possible for you. Once verified, if your plan doesn’t cover the full cost, we can explore various payment options and potential financial assistance.
Get a free, no-obligation insurance verification by calling (844) 491-5566. We’re here to help you every step of the way.
Checking your UnitedHealth Group Insurance Coverage for Drug Rehab is a vital step toward getting the help you need. Here’s a clear list of steps you can take:
It’s a common concern that insurance might not cover the entire cost of addiction treatment, but please don’t let this deter you from seeking help. There are many options available if your UnitedHealthcare plan doesn’t cover the full cost:
The most important thing is to communicate openly with the admissions team at any facility you’re considering. They are experienced in navigating financial complexities and can help you explore all possible avenues to make treatment affordable.
Addiction is a complex, chronic disease, but it is unequivocally treatable. Recovery is not just a dream; it’s a tangible reality for millions of people. Taking the first step, which often involves seeking information about your UnitedHealth Group Insurance Coverage for Drug Rehab, is a courageous and powerful act.
At Sober Steps, we believe that everyone deserves access to quality care. Our platform is built on the principles of confidential and anonymous support. Your privacy is paramount, and we’re here to provide guidance without judgment. We understand the unique challenges faced by individuals and families navigating substance use disorders.
Don’t let questions about insurance or cost prevent you from starting a new chapter. We’re ready to help you understand your benefits, explore your treatment options, and connect you with the resources you need. Call us anytime at (844) 491-5566.
Find the right path to recovery with our help

Discover how addiction is treated with modern therapies. SoberSteps guides you through detox, therapy, and long-term recovery.

Achieve lasting sobriety. Discover key pillars for long term recovery, build strong foundations, and find support with SoberSteps.

Explore SoberSteps abuse programs for addiction recovery. Find treatment options, costs, and support to start your healing journey today.
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.