Need Help Now? How to Connect with a National Addiction Helpline
Get confidential, 24/7 addiction support. Learn how a national addiction helpline guides you to recovery and treatment options.
UMR Health Coverage for Substance Abuse Treatment 2026 provides essential benefits for individuals seeking help with addiction. If you or a loved one is struggling with substance use and has UMR insurance, understanding your coverage is the first critical step toward recovery.
Quick Answer: Does UMR Cover Substance Abuse Treatment in 2026?
Yes. UMR insurance covers various levels of addiction treatment, including:
Coverage levels depend on your specific plan type (HMO vs. PPO), network providers, and employer benefits. Call (844) 491-5566 for a free, confidential benefits check to understand exactly what your plan covers.
What is UMR?
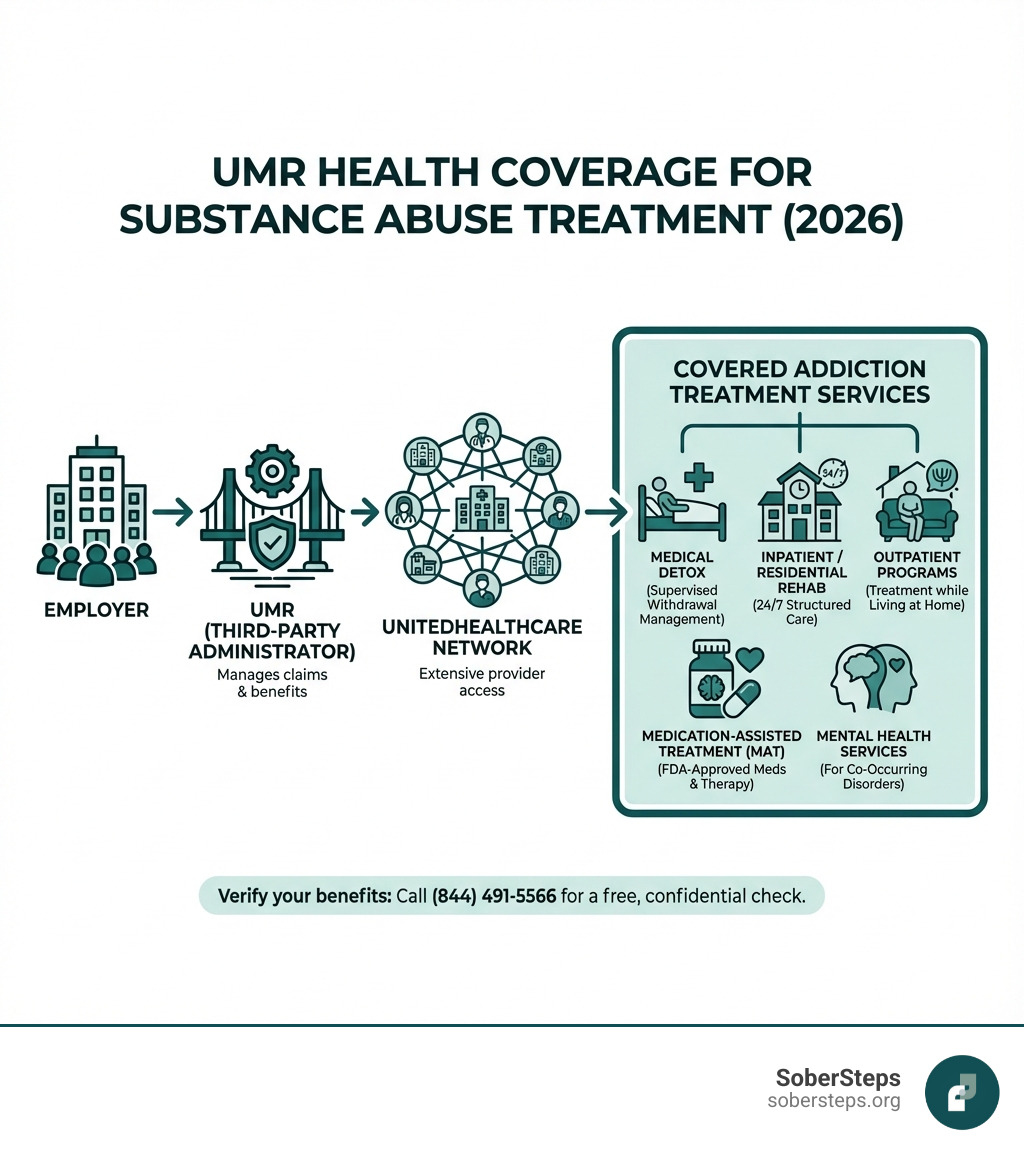
UMR is not an insurance company itself. It’s a third-party administrator (TPA) and a subsidiary of UnitedHealthcare. UMR manages health insurance claims and benefits on behalf of employers. Think of UMR as the bridge between your employer’s health plan and the UnitedHealthcare provider network.
When your employer chooses UMR, you get access to UnitedHealthcare’s extensive network of over 3,000 healthcare providers, including addiction treatment centers. UMR processes your claims, manages pre-authorizations, and ensures you receive the benefits your employer has selected for their health plan.
Why This Matters for Your Recovery
Finding treatment can feel overwhelming, especially when you’re not sure if you can afford it. The good news is that since the Affordable Care Act (ACA) was enacted, all health insurance plans—including those administered by UMR—must cover behavioral health treatment as an essential benefit. This means substance use disorder treatment is no longer optional coverage.
At Sober Steps, we specialize in helping individuals steer insurance coverage for addiction treatment, including UMR Health Coverage for Substance Abuse Treatment 2026, ensuring you get the confidential support you need without financial barriers standing in your way. Our team has helped thousands of people verify their benefits and connect with quality treatment providers.
For immediate assistance, call our 24/7 helpline at (844) 491-5566. Our specialists can verify your UMR benefits in as little as an hour and help you understand your coverage options at no cost to you.
The landscape of health insurance can often feel like a maze, but when it comes to substance abuse treatment, there’s a clear path forward thanks to the Affordable Care Act (ACA). The ACA mandates that all health insurance plans, including those administered by UMR, must include coverage for behavioral health treatment, which encompasses Substance Use Disorder (SUD) services. This means that addiction treatment is considered an “essential health benefit,” ensuring that you have access to the care you need.
UMR, acting as your employer’s third-party administrator, facilitates access to this critical coverage. While specific plan details for 2026 will depend on your employer’s chosen benefits package, the foundational requirement for SUD coverage will remain in place. This is a huge step forward, as historically, addiction treatment was often excluded or had very limited coverage. We understand that deciphering your benefits can be complex, so we’re here to help. For a free, confidential benefits check, we encourage you to call (844) 491-5566 today.
UMR insurance typically covers a comprehensive range of addiction treatment services, reflecting a commitment to supporting individuals through every stage of recovery. This continuum of care is crucial for effective treatment, as addiction is a complex disease requiring varied interventions.
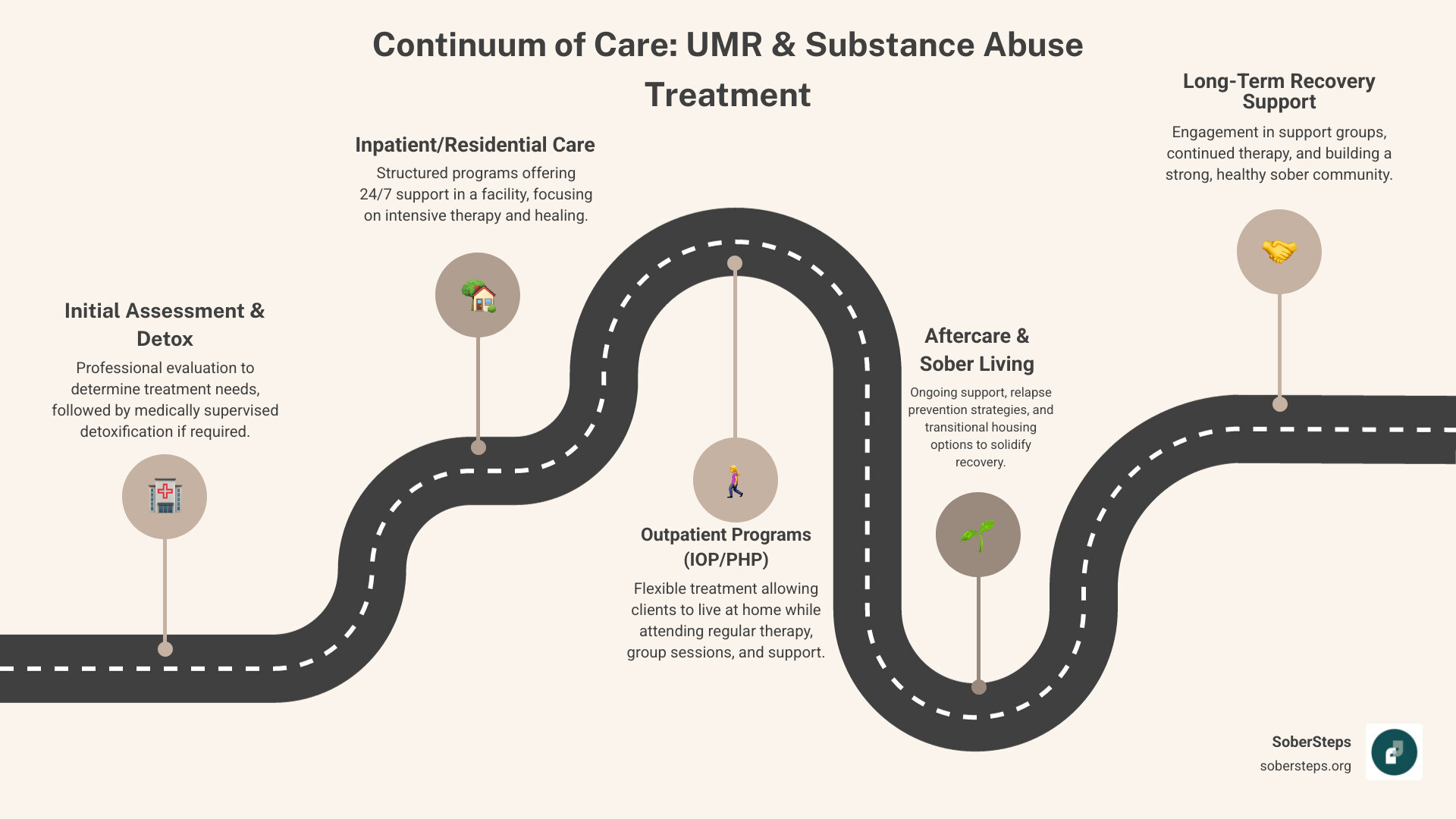
Here’s a breakdown of the types of services you can typically expect UMR Health Coverage for Substance Abuse Treatment 2026 to include:
While UMR facilitates coverage for these services, the exact amount and duration of coverage will depend on your individual plan. We recommend reviewing the Principles of Drug Addiction Treatment from NIDA for a comprehensive understanding of effective treatment approaches.
Yes, absolutely. UMR insurance often covers both substance use disorder and co-occurring mental health services. This is a critical aspect of effective treatment, as addiction rarely exists in a vacuum. Many individuals struggling with substance abuse also contend with underlying mental health conditions such as anxiety, depression, bipolar disorder, or trauma. These are often referred to as “dual diagnoses.”
UMR, in alignment with best practices in behavioral health, emphasizes an integrated care model. This means that treatment addresses both the addiction and any co-occurring mental health disorders simultaneously. This holistic approach leads to better treatment outcomes, as treating one without the other often results in relapse for both conditions.
UMR’s commitment to expanding mental health opportunities ensures that services like individual therapy, group counseling, psychiatric evaluations, and medication management for mental health conditions are typically covered. Their network includes specialists for the treatment of mental or emotional health concerns, ensuring you receive comprehensive care. For more detailed information on this important topic, you can refer to the Information on co-occurring disorders from SAMHSA.

Understanding your UMR Health Coverage for Substance Abuse Treatment 2026 involves more than just knowing what’s covered; it also means understanding how to access those benefits. This includes processes like benefit verification, pre-authorization, understanding medical necessity, and potential referral requirements. These steps ensure that the treatment you receive is appropriate, covered by your plan, and delivered by qualified providers.
We know this part can feel like a lot of paperwork and phone calls, but we’re here to simplify it. Call (844) 491-5566 to understand your plan’s specific requirements, and we can help you steer these often-confusing steps.
The type of UMR plan you have—whether it’s an HMO (Health Maintenance Organization) or a PPO (Preferred Provider Organization)—significantly impacts your coverage for substance abuse treatment, particularly regarding provider networks and out-of-pocket costs.
HMO Plans:
PPO Plans:
Here’s a quick comparison:
| Feature | UMR HMO Plan | UMR PPO Plan |
|---|---|---|
| Provider Network | Primarily in-network providers | In-network and out-of-network providers |
| PCP Referral | Often required for specialists/treatment | Generally not required |
| Out-of-Network | Little to no coverage | Covered, but at a higher out-of-pocket cost |
| Premiums | Generally lower | Generally higher |
| Flexibility | Less | More |
| Cost Savings | Higher savings when staying in-network | Savings for in-network, some coverage for out-of-network (up to 30% off) |
| Continuity of Care | May require specific forms for out-of-network care | More straightforward for out-of-network, but still requires verification |
It’s crucial to understand your specific plan’s details. If you have an HMO, ensure the treatment facility is in-network or be prepared for significantly higher costs. For PPO plans, while you have more choice, confirming coverage and potential out-of-pocket expenses for out-of-network providers is still a smart move. In some cases, a Continuity of Care form may allow for continued coverage with an out-of-network facility, but approval is not guaranteed.
Even with robust UMR Health Coverage for Substance Abuse Treatment 2026, you’ll likely encounter some out-of-pocket costs. These are standard components of most insurance plans and include:
The exact amount you’ll pay depends heavily on your specific UMR plan, the type of treatment you receive, and whether you choose in-network or out-of-network providers. Preventative care is always 100% covered when it’s within the UnitedHealthcare Choice Plus network.
We know it can be a lot to keep track of, but understanding these terms is vital to planning your treatment without financial surprises. For a clear breakdown of your potential costs and to verify your specific plan’s details, call (844) 491-5566. Our specialists can help clarify your financial responsibilities.
Finding a rehab center that accepts your UMR Health Coverage for Substance Abuse Treatment 2026 is a crucial step toward recovery. We want to make this process as straightforward as possible for you.
Here’s how to approach finding and accessing UMR-accepting facilities:
Benefits of Using Insurance vs. Self-Pay: Using your UMR insurance for addiction treatment offers significant advantages compared to paying out-of-pocket. It can dramatically reduce your financial burden, making life-saving treatment accessible. With UMR’s extensive network through UnitedHealthcare, you can access quality, evidence-based care that might otherwise be unaffordable. This allows you to focus on your recovery rather than worrying about mounting bills.
We understand that finding the right facility can be daunting. For confidential help finding a UMR-accepting facility that meets your needs, call (844) 491-5566. Our team can assist you in connecting with appropriate treatment options.
While the core principles of UMR Health Coverage for Substance Abuse Treatment 2026 will remain consistent due to federal mandates, the specifics of your policy can vary. Here’s what you should keep in mind:
We understand you likely have many questions about using your UMR insurance for addiction treatment. Here, we address some of the most common inquiries.
Verifying your UMR benefits is a crucial step to ensure you understand your coverage and potential costs. We recommend a few reliable methods:
For immediate, confidential help with verifying your UMR benefits and understanding your options, call our 24/7 helpline at (844) 491-5566. We’re here to assist you every step of the way.
It’s common for insurance plans, including UMR, not to cover 100% of addiction treatment costs. If you find yourself in this situation, don’t despair—you still have options:
The most important thing is not to let financial concerns deter you from seeking help. There are almost always solutions available.
Yes, UMR often requires pre-authorization for certain types of substance abuse treatment, especially for more intensive levels of care like inpatient or residential rehabilitation.
Failing to obtain required pre-authorization can result in your claim being denied, leaving you responsible for the full cost of treatment. Therefore, always confirm pre-authorization requirements with your provider or UMR before starting any intensive treatment program.
Navigating the complexities of insurance can feel overwhelming, especially when you’re seeking help for something as personal and critical as substance abuse. However, with UMR Health Coverage for Substance Abuse Treatment 2026, you have a powerful tool to access the care you need. We’ve seen how UMR, as a dedicated third-party administrator for UnitedHealthcare, works to connect you with a vast network of providers, ensuring that essential behavioral health benefits are within reach.
The Affordable Care Act guarantees coverage for substance use disorder treatment as an essential benefit, making affordable treatment a reality for many. By understanding your plan’s specifics, whether it’s an HMO or PPO, and by actively verifying your benefits, you can significantly reduce your out-of-pocket costs and focus on what truly matters: your recovery.
Empowerment through knowledge is your greatest asset on this journey. You don’t have to face this alone. SoberSteps is committed to providing confidential, anonymous assistance, helping you understand your UMR benefits and connect with treatment options that accept your insurance. Your recovery journey starts with a simple, private conversation.
We encourage you to take that vital first step. Verify your insurance coverage now to speak with a specialist who can help clarify your UMR benefits and guide you toward a path of lasting recovery. We are here, ready to help.
Get confidential, 24/7 addiction support. Learn how a national addiction helpline guides you to recovery and treatment options.
Discover safe, medically supervised withdrawal. Learn what an inpatient detox program offers for your first step to lasting recovery.

Find free rehab centers near me with 5 genius hacks. Overcome financial barriers & start your recovery journey today.
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.