
Beyond the Brain: Unlocking Effective Addiction Treatment Options
Understand addiction as a treatable brain condition. Explore effective addictions treatment options, therapies, and find your path to recovery.
Relapse Prevention is a critical set of skills and strategies that helps individuals maintain sobriety and avoid returning to substance use after treatment. If you’re seeking information on relapse prevention, here’s what you need to know right away:
Core Elements of Relapse Prevention:
Important Reality: Research shows that relapse rates are approximately 50% within the first 12 weeks after completing intensive inpatient programs. This isn’t a sign of failure—addiction is a chronic disease, and relapse can be a common part of the recovery process. The key is having proactive strategies in place.
Recovery is a journey, not a destination. It requires ongoing commitment, self-awareness, and the right support system. The good news? With the right tools and a solid relapse prevention plan, you can significantly reduce your risk and build a fulfilling life in sobriety.
If you’re struggling right now and need immediate, confidential support, call us at (844) 491-5566. Our compassionate team is available 24/7 to help you find the treatment and resources you need.
At Sober Steps, we understand the challenges of maintaining recovery because we’ve dedicated ourselves to providing confidential, anonymous support for individuals navigating mental health and substance use disorders. Our comprehensive approach to Relapse Prevention connects you with evidence-based strategies, treatment resources, and a supportive community to help you succeed at every stage of your recovery journey.
When we talk about relapse, it’s easy to picture a sudden, dramatic event. However, this isn’t usually the case. Relapse is almost always a progressive process, not an abrupt incident. Think of it like a winding road with clear warning signs along the way. Pioneering work by G. Alan Marlatt and Terence Gorski has helped us understand this process, allowing us to intervene much earlier.
A crucial distinction in Relapse Prevention is understanding the difference between a “lapse” and a “relapse.” A lapse, sometimes called a “slip-up,” is a single instance of substance use after a period of abstinence. It’s like taking one wrong turn on our winding road. A relapse, on the other hand, implies a return to a previous, uncontrolled pattern of substance use—it’s getting completely lost and heading back to square one.
The way we respond to a lapse is critical. Viewing a lapse as an absolute failure can trigger the “Abstinence Violation Effect” (AVE), where guilt and shame lead to further use. Instead, we encourage viewing a lapse as a learning opportunity, a chance to identify what went wrong and adjust our plan to prevent a full-blown relapse. It’s a chance to re-evaluate, strengthen our coping skills, and get back on track.
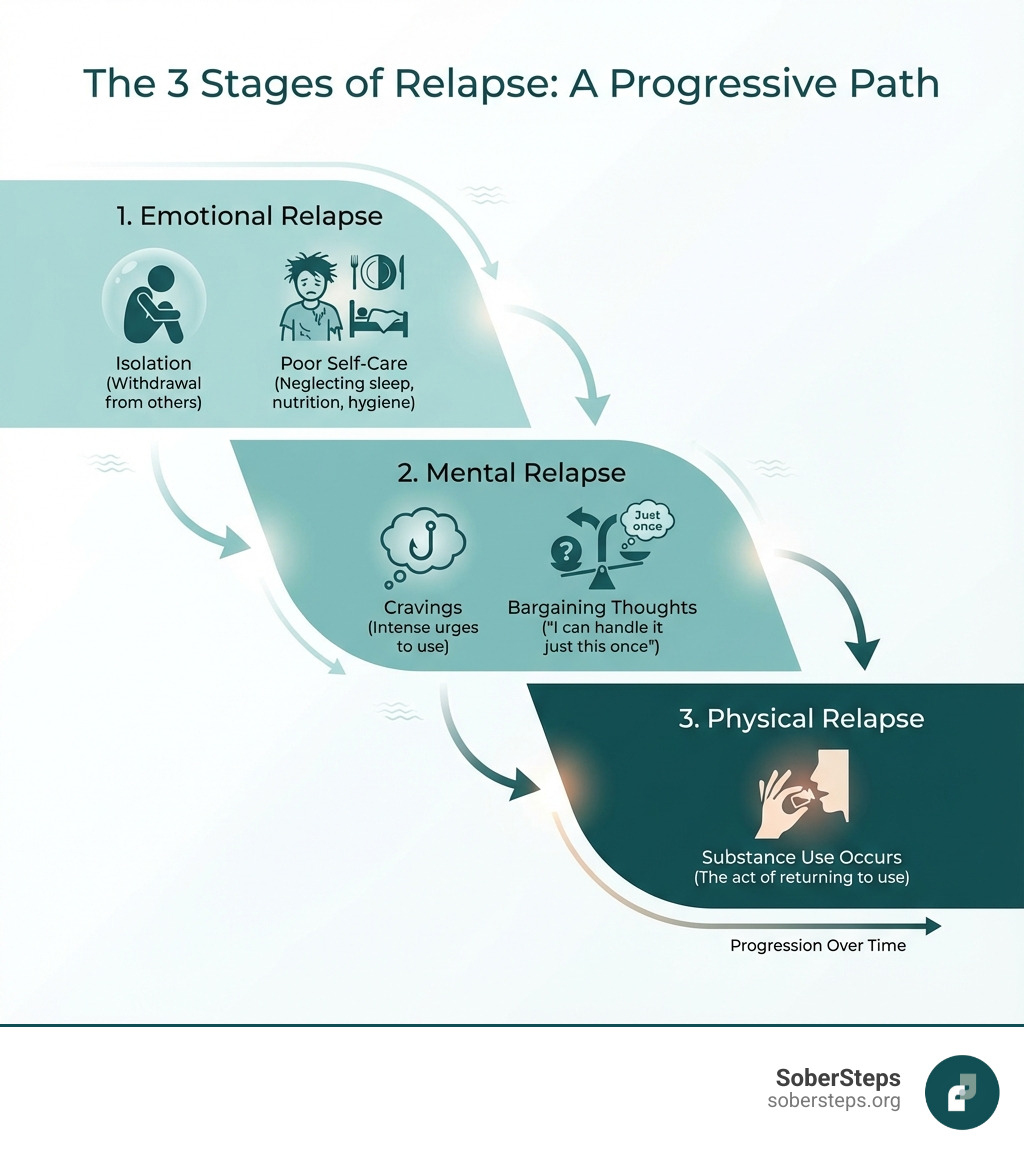
Relapse unfolds in distinct stages, often starting long before any substance is consumed. Recognizing these stages is paramount for effective Relapse Prevention.
1. Emotional Relapse: This is the earliest stage, where individuals aren’t actively thinking about using but their emotions and behaviors are setting the stage for future vulnerability. The common denominator here is often poor self-care. – Signs: Bottling up emotions, isolating from others, poor eating habits, irregular sleep, neglecting self-care, feeling overwhelmed, anxiety, anger, irritability, defensiveness, not asking for help, and neglecting recovery routines like attending meetings. We might start to feel “HALT” – Hungry, Angry, Lonely, or Tired – which are prime conditions for emotional instability.
2. Mental Relapse: At this stage, there’s an internal battle. The individual starts contemplating substance use. – Signs: Cravings for substances become more frequent or intense, thinking about people, places, or things associated with past use, glamorizing past use (forgetting the negative consequences), minimizing the severity of past problems, bargaining with oneself (“just one time”), lying to others or oneself about thoughts and actions, and actively planning a relapse. This stage involves a significant internal struggle between the desire to use and the desire to remain abstinent.
3. Physical Relapse: This is the final stage, where the individual actually consumes the substance. – Signs: This stage is marked by the act of using drugs or alcohol. It often begins with a lapse, which, if not addressed quickly and effectively, can escalate into a full return to previous patterns of substance use.
A significant and often underestimated risk factor for relapse, especially in early recovery, is Post-Acute Withdrawal Syndrome (PAWS). While acute withdrawal symptoms subside after detoxification, PAWS can linger for an extended period, sometimes up to 2 years.
PAWS symptoms are unpredictable and can include:
The unpredictable nature and discomfort of PAWS symptoms can make individuals feel like they aren’t progressing, leading to frustration and increased vulnerability to relapse. Learning to identify and manage PAWS symptoms through therapy, self-care, and support is a crucial aspect of early Relapse Prevention.
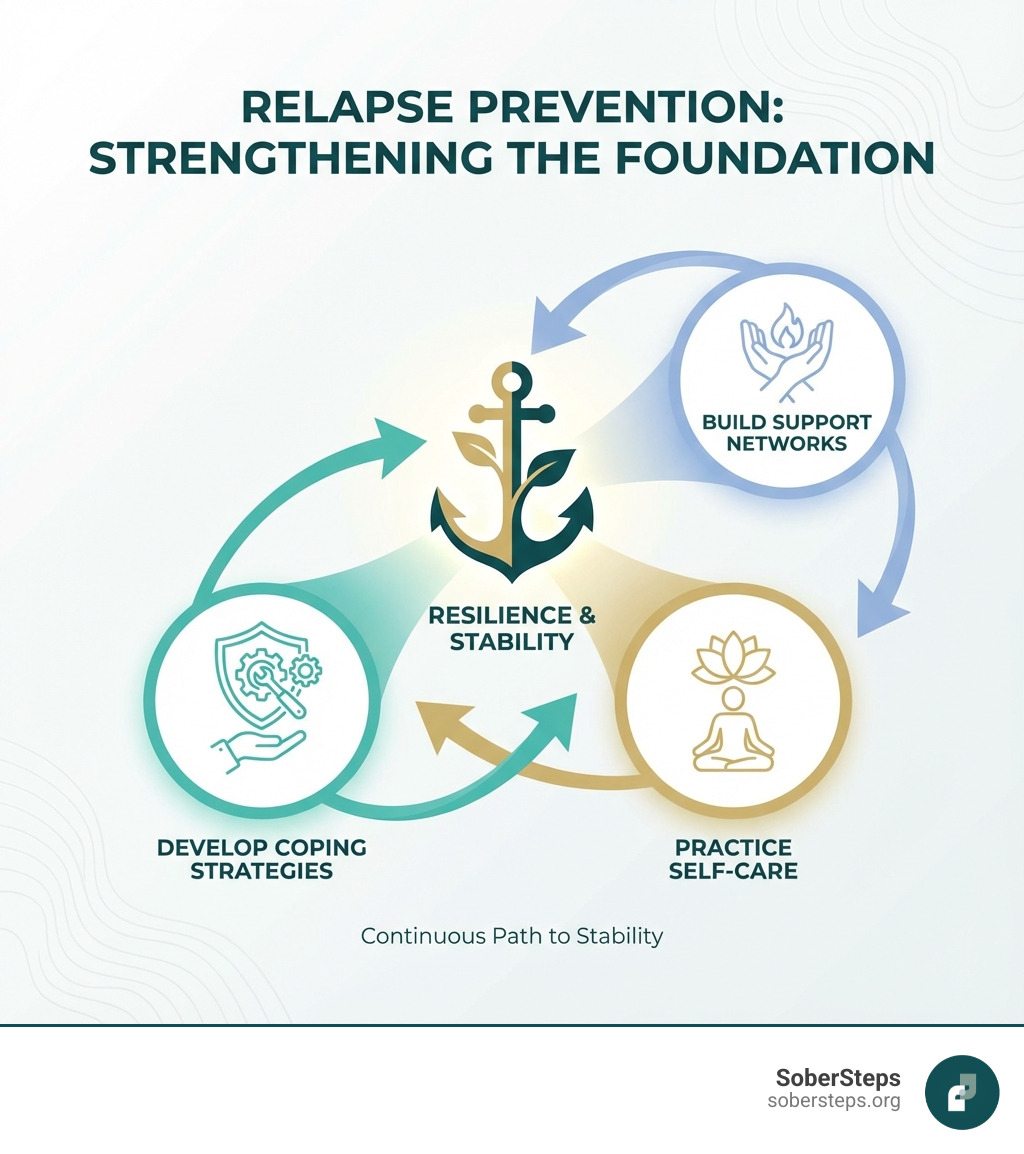
Effective Relapse Prevention isn’t about having a magic shield; it’s about building a robust defense system. This involves a proactive approach, anticipating challenges and equipping ourselves with the tools to steer them, rather than reacting only when a crisis hits. Taking personal responsibility for our recovery means actively engaging in strategies that support our sobriety. For immediate, anonymous support, call (844) 491-5566.
Triggers are like tripwires that can set off cravings or thoughts of using. They can be internal or external, and identifying them is the first step in disarming them.
A useful tool for identifying internal triggers is the HALT acronym:
Creating a “trigger inventory” is a highly effective Relapse Prevention strategy. This involves writing down every internal and external trigger you can identify and, for each, listing healthy coping mechanisms or avoidance strategies.
Dr. Stephen M. Melemis outlined “The Five Rules of Recovery” in the Yale Journal of Biology and Medicine, providing a simple yet powerful framework for maintaining sobriety. These rules guide individuals in making choices that support long-term recovery.
For a deeper dive into these rules, you can refer to the Yale Journal article on the Five Rules of Recovery.
No one recovers alone. Building a strong and diverse support network is a cornerstone of effective Relapse Prevention.
Our compassionate team at SoberSteps can help you explore options and connect with the right support system for your journey; call us for confidential support at (844) 491-5566.
While personal commitment and peer support are vital, professional treatment offers evidence-based therapies and techniques that significantly improve the chances of long-term recovery. Combining these professional strategies with personal efforts creates a powerful framework for Relapse Prevention. Our team is available 24/7 at (844) 491-5566 to guide you through these options.
Several therapeutic approaches have strong empirical support for their effectiveness in Relapse Prevention:
Integrating mind-body practices can dramatically improve emotional regulation, reduce stress, and help manage cravings, all crucial elements of Relapse Prevention.
These techniques help individuals develop a sense of “comfort with discomfort,” understanding that negative feelings are normal and don’t necessarily require a substance to cope.
For many, medication-assisted treatment (MAT) is a vital component of Relapse Prevention, especially for alcohol and opioid use disorders. These medications, when prescribed and monitored by a healthcare professional, can reduce cravings, block the effects of substances, and help maintain abstinence.
Here’s a quick comparison of common medications for Alcohol Use Disorder:
| Medication | Mechanism of Action | Primary Benefit | Efficacy Notes |
|---|---|---|---|
| Disulfiram | Blocks alcohol metabolism, causing unpleasant reaction | Deterrent to drinking | Superior when used in observed dosing. |
| Naltrexone | Blocks opioid receptors, reduces cravings | Reduces cravings, blocks euphoric effects | NNT = 20 to prevent return to any drinking. |
| Acamprosate | Restores neurotransmitter balance | Reduces post-acute withdrawal symptoms | NNT = 12 to prevent return to any drinking. |
Note: There is limited or insufficient evidence for specific medications for cannabis and methamphetamine relapse prevention.
Recovery is a dynamic journey, not a static state. It’s a process of personal growth with developmental milestones, each presenting its own unique challenges and risks for relapse. Understanding these stages allows us to tailor our Relapse Prevention strategies over time.
The abstinence stage, typically lasting 1 to 2 years, is often the most challenging and relapse-prone period. The brain is still healing, and individuals are learning to steer life without substances.
Lasting approximately 2 to 3 years, the repair stage shifts focus from initial abstinence to healing and rebuilding.
The growth stage typically begins 3 to 5 years after stopping substance use and is a lifetime path. While the immediate threat of relapse may lessen, new challenges emerge.
A comprehensive, written Relapse Prevention plan is your personal roadmap for navigating the challenges of recovery. It’s not just a good idea; it’s a vital tool that can literally save your life. This plan should be accessible, reviewed regularly, and custom precisely to your unique triggers, strengths, and support systems. Need help creating a plan? Call our confidential line at (844) 491-5566.
A well-crafted Relapse Prevention plan is a living document that evolves with your recovery. Here are the essential elements we recommend including:
Creating the plan is only half the battle; implementing it consistently is where the magic happens.
Recovery is not merely the absence of substance use; it’s the presence of a fulfilling, meaningful life. While the path to sobriety can be challenging, we firmly believe that recovery is possible for everyone. Relapse Prevention is not about avoiding failure; it’s about acquiring a robust set of skills and strategies that empower you to steer life’s inevitable ups and downs without resorting to old patterns.
A proactive, personalized Relapse Prevention plan is your best defense, providing a clear roadmap and a powerful toolkit for maintaining your sobriety. It embodies hope and empowerment, reminding you that you have the strength and the resources to face any challenge.
At SoberSteps, we are dedicated to supporting you every step of the way. We provide a confidential and anonymous platform to help you find the help you need, connecting you with evidence-based treatments and a community that understands. Don’t let fear or uncertainty hold you back from the life you deserve. Take the first step towards lasting recovery by calling (844) 491-5566 or visiting our website. Your journey to a healthier, happier future starts now.
Find confidential support for addiction today or call (844) 491-5566

Understand addiction as a treatable brain condition. Explore effective addictions treatment options, therapies, and find your path to recovery.

Explore SoberSteps abuse programs for addiction recovery. Find treatment options, costs, and support to start your healing journey today.

In crisis? Get immediate addiction help now. Call 911, 988, or SoberSteps for urgent support & treatment guidance.
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.