Understanding Mental Institutions and Psychiatric Hospitals Today
A mental institution, more commonly known today as a psychiatric hospital or behavioral health facility, is a specialized medical facility that provides intensive treatment for individuals experiencing severe mental health crises or persistent mental illness. If you’re searching for information about mental institutions, here’s what you need to know:
What Mental Institutions Provide:
- Crisis Stabilization – Immediate safety and assessment for acute psychiatric emergencies
- Inpatient Psychiatric Care – 24/7 medical supervision with medication management and therapy
- Residential Treatment – Extended care for severe and persistent mental illness
- Specialized Programs – Targeted treatment for specific populations (children, adolescents, adults, veterans)
- Dual Diagnosis Treatment – Integrated care for co-occurring mental health and substance use disorders
The term “mental institution” carries historical weight. These facilities have evolved dramatically from the asylums of the past—places of isolation and custody—into modern recovery-focused treatment centers. Today’s psychiatric hospitals emphasize evidence-based treatment, patient rights, and community reintegration rather than long-term confinement.
According to recent data, 22.8% of U.S. adults (58.7 million people) experienced mental illness in the past year, and approximately one-third of those individuals also had a co-occurring substance use disorder. Yet stigma and confusion about psychiatric hospitals often prevent people from seeking the help they desperately need.
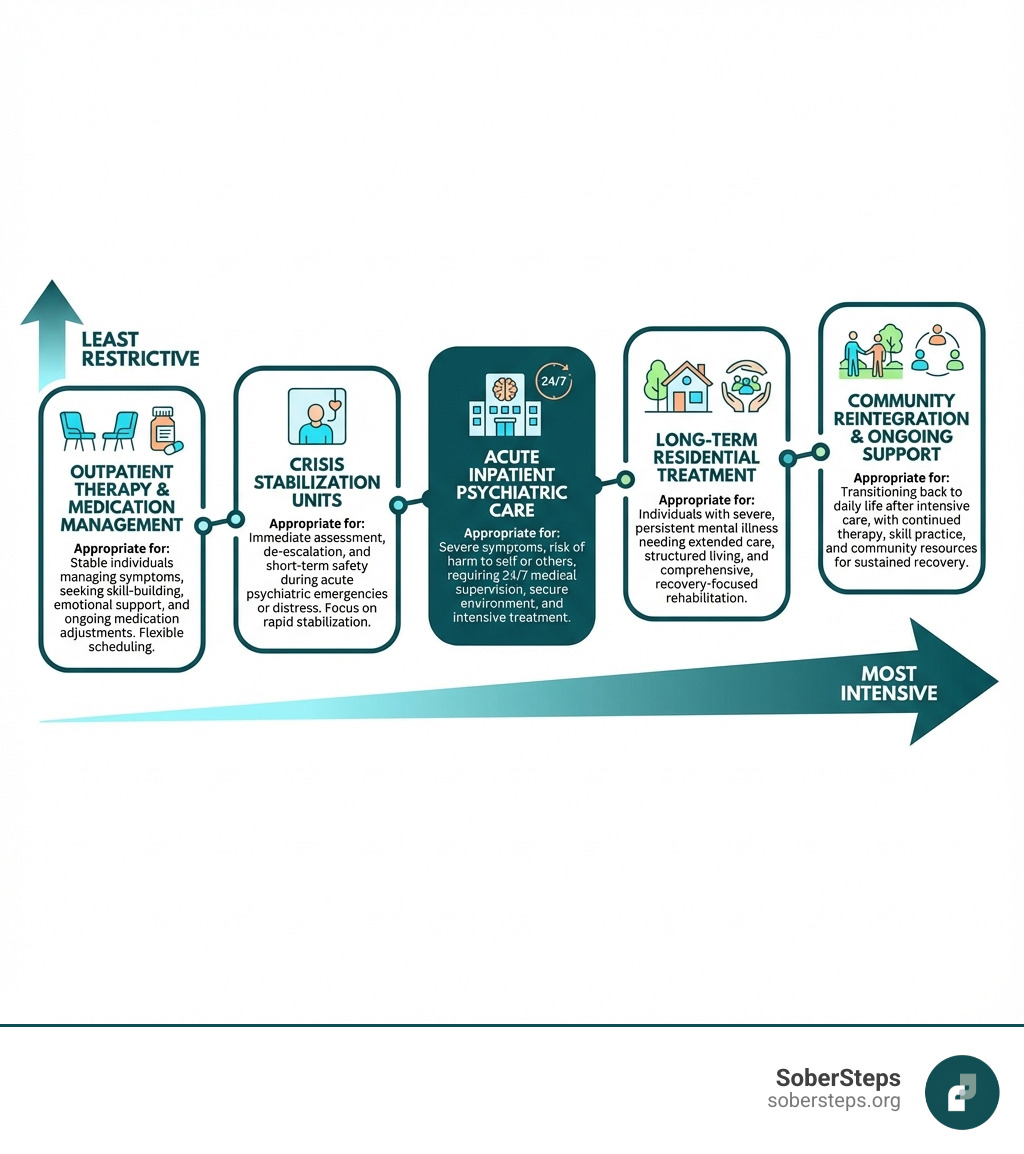
Modern mental health care exists on a continuum—from outpatient therapy and medication management to intensive inpatient hospitalization. Understanding this spectrum helps individuals and families find the right level of care. Whether someone is experiencing their first mental health crisis or managing a long-term condition, psychiatric hospitals play a vital role in the treatment ecosystem.
You are not alone, and seeking help is a sign of strength, not weakness. Recovery is possible with the right support and treatment. If you or someone you love is struggling, confidential help is available 24/7 by calling (844) 491-5566.
At Sober Steps, we’ve dedicated ourselves to guiding individuals through the complex landscape of mental health and substance use treatment, connecting people with the psychiatric care and resources they need. We understand the challenges surrounding mental institutions and are here to provide anonymous, judgment-free support as you steer your options.
Terms related to mental institution:
The Evolution of the Modern Psychiatric Hospital
When we hear the phrase “mental institution,” images from old movies or historical accounts might come to mind, often depicting places of despair and confinement. But the journey of these facilities, from their earliest forms to the modern psychiatric hospitals we know today, is a fascinating story of evolving understanding, changing societal attitudes, and medical advancements. The fundamental shift has been from a model of custody and restraint to one focused on care, recovery, and reintegration into the community.
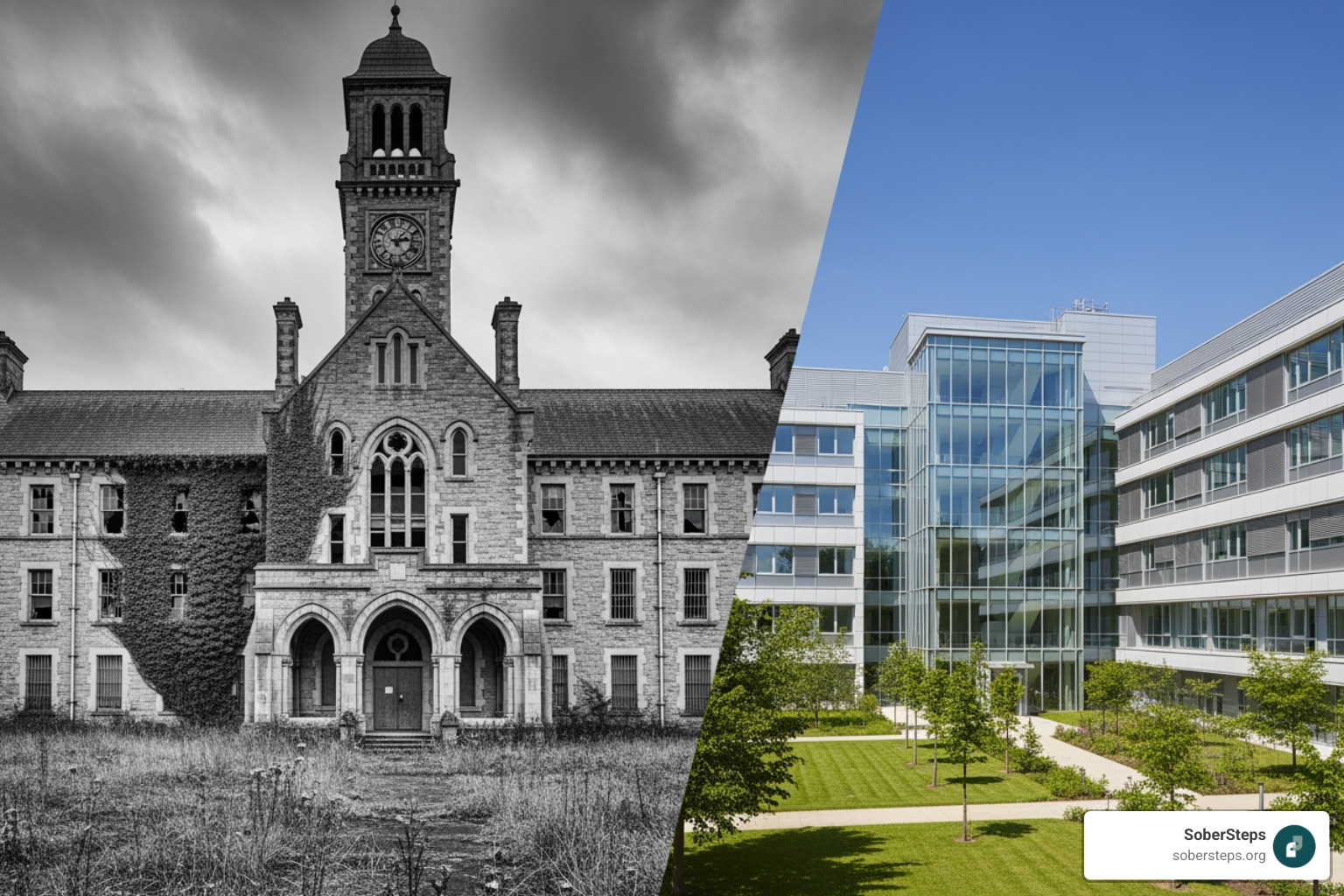
This change is often called deinstitutionalization, a movement that gained significant momentum in the United States during the mid-20th century. It led to a rise in community-based care, with an emphasis on helping individuals manage their conditions while living more independently. The ultimate goal is to foster recovery and reintegration, ensuring that treatment supports a fulfilling life outside the hospital walls.
From Asylums to Recovery-Focused Care
The earliest forms of mental institution care were often rudimentary and, by today’s standards, inhumane. In the medieval era, those considered “mad” might be housed in cages, compelled to amuse royalty, or simply kept within city walls. The Islamic world, however, offered a contrasting approach with institutions called Bimaristans, which provided care and even music therapy for the insane as early as 918 CE in Baghdad.
In Europe, institutions like London’s notorious Bethlem Royal Hospital, often referred to as “Bedlam,” began as charitable hospitals but became synonymous with the brutal treatment and public spectacle of mental illness. By the 18th century, private madhouses proliferated, and the “trade in lunacy” became a well-established business in Britain.
A significant turning point came with the moral treatment movement in the late 18th and early 19th centuries. Figures like Philippe Pinel in France and William Tuke in England advocated for more compassionate and rational care, emphasizing rehabilitation and minimizing physical restraints. In the United States, Dorothea Dix was a tireless advocate for the mentally ill, campaigning for the establishment of state-funded asylums with more humane conditions. Her efforts led to the creation of numerous state psychiatric hospitals across the country.
The mid-20th century brought further reforms and the impact of psychotropic medications. The introduction of antipsychotic drugs like chlorpromazine in the 1950s and other medications, such as those used in the history of lithium therapy, dramatically altered the landscape of mental health treatment. These pharmacological breakthroughs made it possible for many patients to manage their symptoms more effectively, leading to higher discharge rates and a shift away from long-term institutionalization toward community-based care.
Criticisms and Controversies Surrounding the Mental Institution
Despite the progress, the history of the mental institution is also marked by significant criticisms and controversies. Sociologist Erving Goffman famously described mental hospitals as “Total Institutions” in his 1961 work, arguing that they were places where a person’s entire life was confined and controlled, similar to prisons or concentration camps. This concept highlighted the dehumanizing aspects of institutional life and contributed to a broader critique of traditional psychiatric care.
Stigma and public perception have always been major challenges. For centuries, mental illness was misunderstood and feared, leading to the isolation and marginalization of those affected. Even today, despite increased awareness, the stigma associated with psychiatric care can prevent individuals from seeking help.
Debates around involuntary commitment remain a sensitive issue. While involuntary admission criteria generally require a person to be a danger to themselves or others, concerns about patient autonomy and potential abuse persist. We value a patient’s right to choose their treatment, but sometimes, for safety, involuntary commitment is a necessary step. Scientific research on involuntary mental health treatment continues to explore the ethical and practical implications of such interventions.
The use of restraints and seclusion has also been a contentious practice. While modern psychiatric hospitals aim to minimize these interventions, they are sometimes used as a last resort to ensure patient and staff safety during acute crises. Historically, however, these methods were often overused and abused.
Perhaps one of the darkest chapters in the history of mental institutions is the political abuse of psychiatry, where mental health diagnoses were used to suppress political dissent in some countries. This stark reminder underscores the importance of robust patient rights and ethical oversight in all psychiatric care settings.
Types of Psychiatric Hospitals and Levels of Care
Modern mental health care operates on a spectrum, recognizing that different individuals require varying intensities and durations of treatment. Matching the right level of care to individual needs is crucial for effective recovery. Psychiatric hospitals, or mental institutions, offer a diverse range of inpatient services, from very short-term crisis interventions to extended residential programs. For help finding the right level of care, call (844) 491-5566.
Crisis Stabilization Units (CSUs)
Crisis Stabilization Units (CSUs) are designed for individuals experiencing acute psychiatric episodes. These units provide immediate safety and assessment in a secure environment. The primary goal is to stabilize the crisis, often involving suicide prevention, medication initiation or adjustment, and a thorough evaluation of the individual’s mental state. Stays in CSUs are typically very short, ranging from 24 to 72 hours, after which patients are linked to appropriate ongoing care, which might be an inpatient hospital, residential treatment, or outpatient services. In the United States, high acuity crisis stabilization units serve individuals who are actively suicidal, violent, or intoxicated.
Inpatient Psychiatric Hospitals
Inpatient psychiatric hospitals offer a more structured and extended level of care than CSUs. These facilities can be stand-alone psychiatric hospitals or psychiatric units located within general hospitals. They provide a therapeutic environment with 24/7 medical supervision.

Here, patients receive comprehensive treatment, including medication management, individual therapy, and group therapy sessions. Group therapy, as pictured above, is a common and effective modality, allowing patients to share experiences and develop coping skills in a supportive setting. The goal of inpatient care is to stabilize acute symptoms, provide intensive treatment, and develop a robust discharge plan for continued recovery. Conditions treated often include schizophrenia, bipolar disorder, major depressive disorder, eating disorders, and severe anxiety.
Long-Term Care and Residential Treatment
For individuals with severe and persistent mental illness (SPMI) or complex conditions that require prolonged support, long-term care and residential treatment programs are available. These facilities offer extended stays, often lasting months or even longer, providing a higher level of support and care compared to acute inpatient settings.
Residential treatment centers focus on comprehensive support, heavy monitoring, and life skills training to help patients achieve greater independence. This can include vocational training, educational support, and social skills development. The ultimate goal remains community reintegration, helping individuals transition back to a less restrictive environment with the skills and confidence needed to thrive. These long-term psychiatric care options are designed to provide comprehensive support over an extended period, focusing on holistic recovery.
Navigating Treatment and Accessing Help
Understanding the mental health landscape can feel overwhelming, especially when you or a loved one is in distress. However, numerous public and private options are available to help you access the care you need. Finding specialized programs that cater to specific populations and needs is key to effective treatment. If you need help, call our 24/7 line at (844) 491-5566.
Specialized Programs for Diverse Populations
Modern psychiatric care recognizes that different age groups and demographics have unique needs. Many mental institution facilities and programs offer specialized services:
- Children’s Mental Health Services (ages 5-12): These programs address emotional and behavioral problems in younger children, such as impulsive or defiant behaviors, inability to concentrate, extreme mood swings, or physical aggression. Treatment often involves family therapy and play therapy.
- Adolescent Inpatient and Outpatient Programs: Teens face unique challenges, and specialized programs build treatment plans based on individual needs. These can include inpatient care, day treatment, and intensive outpatient programs for mental health and substance use disorders.
- Adult Psychiatric Care: Comprehensive treatment options are available for adults suffering from a wide range of mental health disorders, including inpatient care, dual diagnosis care, partial hospitalization, and intensive outpatient programs.
- Veteran and Military Programs: Many facilities offer quality behavioral health services for veterans and active duty service members, including inpatient and outpatient programs to treat mental health, substance use, and dual diagnosis issues.
- Dual Diagnosis Treatment: Given that approximately one-third of adults with mental illness also have a co-occurring substance use disorder, integrated treatment for both conditions is crucial. These programs address both the mental health disorder and the substance use disorder simultaneously.
The Role of State and Local Mental Health Services
In the United States, state and local governments play a significant role in providing mental health care, particularly for individuals who are uninsured, underinsured, or otherwise unable to pay.
State-funded psychiatric hospitals are operated by state health and human services departments. For example, the Texas Health and Human Services system operates nine state hospitals that provide services for adults, children, and individuals involved with the justice system who have mental health issues. These facilities are typically Medicare-certified, Medicaid-approved, and accredited by The Joint Commission, ensuring a standard of quality care.
The Texas Statewide Behavioral Health Strategic Plan outlines a coordinated approach to behavioral health services across the state. This plan involves various entities working together to ensure comprehensive care.
Local Mental Health Authorities (LMHAs) or Local Behavioral Health Authorities (LBHAs) are critical entry points into the public mental health system. They routinely screen all requests for voluntary admission to state facilities, ensuring that hospitalization is the least restrictive treatment alternative. They also provide important patient facts to the facility and have the final authority on admission to state hospitals. This system strives to ensure that individuals receive care in the most appropriate and least restrictive setting possible.
The Admission Process to a Mental Institution
Understanding the admission process to a mental institution or psychiatric hospital can alleviate some anxiety during a difficult time. Whether you’re seeking help for yourself or a loved one, knowing the pathways to admission, financial considerations, and patient protections is crucial.
Admission Criteria: Voluntary vs. Involuntary
There are generally two main pathways to admission:
-
Voluntary Admission: This occurs when an individual willingly seeks treatment and agrees to be admitted to a psychiatric hospital. The appropriate LMHA routinely screens all requests for voluntary admission to ensure hospitalization is the least restrictive treatment alternative. No person is denied voluntary admission without thorough documentation and appropriate referral, as recommended by the screening physician. Patients admitted voluntarily retain the right to request discharge, though facilities may have a process to evaluate the safety of such a request.
-
Involuntary Commitment: This happens when an individual is admitted to a psychiatric hospital without their consent. In general, to be involuntarily admitted, a person must show symptoms of mental illness and that they are a danger to themselves or others. This can include suicidal ideation, self-harm, or threats of violence toward others. Emergency detention orders allow for short-term involuntary holds (e.g., 72 hours) to stabilize the individual and conduct a thorough psychiatric evaluation. A physician’s screening is essential to determine if the criteria for involuntary commitment are met. The guiding principle is always the “least restrictive treatment alternative,” meaning involuntary commitment is only used when less restrictive options are insufficient to ensure safety.
For individuals involved with the justice system, forensic admissions are also a pathway. If a judge rules a defendant incompetent to stand trial, an order for competency-restoration is issued, and the state hospital system manages the admission to a specialized facility.
Understanding Costs and Insurance Coverage
The costs associated with psychiatric treatment can be a significant concern, but various options exist to make care accessible.
- Private Insurance Plans: Most private health insurance plans cover mental health and substance use disorder treatment, often mandated by parity laws. It’s important to verify your specific benefits with your insurance provider. We can help you steer this complex landscape; simply call (844) 491-5566 to verify your insurance benefits confidentially.
- Medicare and Medicaid: State hospital facilities in the U.S. are typically Medicare-certified and Medicaid-approved. Medicaid often offers more complete coverage of mental health services than private insurance, especially for those under 65. If you have lost your Medicaid coverage, information on re-enrolling in Texas Medicaid (and similar programs in other states) is available.
- Sliding Scale Fees and Financial Assistance: Many providers are committed to providing care to persons who are uninsured, underinsured, or otherwise unable to pay. They offer discounted/sliding fee schedules based on family size and income, ensuring that financial capacity does not prevent access to quality care. No one will be denied access to services due to inability to pay.
- No Surprises Act: This federal act protects patients from unexpected medical bills, particularly for out-of-network services received in an emergency or from an out-of-network provider at an in-network facility.
On average, hospital stays for mental health and substance use disorders in the U.S. can cost around $1,400 per day, with most stays lasting about 6 days, totaling an average of $7,100. However, these costs vary widely based on the specific condition and length of stay. For instance, admissions for eating disorders can last around 14 days and cost about $19,400, while schizophrenia treatment might be around $8,900 over 11 days.
Your Rights as a Patient in a Mental Institution
Patients in a mental institution retain fundamental rights, which are protected by law and ethical guidelines. These rights ensure that individuals are treated with dignity, respect, and receive appropriate care.
- Right to be treated with dignity: All patients have the right to humane treatment and respect for their personal integrity.
- Right to informed consent: Patients must be fully informed about their treatment plan, including potential risks and benefits, and have the right to consent or refuse treatment (unless legally deemed incompetent or in involuntary commitment situations where treatment is court-ordered for safety).
- Confidentiality and HIPAA: Patient information is protected under HIPAA (Health Insurance Portability and Accountability Act), ensuring privacy and confidentiality of medical records.
- Communication with family and legal counsel: Patients generally have the right to communicate with their family members, significant others, and legal representatives, though facilities may have policies regarding timing and methods to maintain a therapeutic environment.
- Patient advocates: Patients have the right to access patient advocates who can help them understand their rights, voice concerns, and steer the treatment system.
- Filing a complaint: If a patient or their family believes their rights have been violated or they have received substandard care, they have mechanisms to file a complaint, including directly with the facility, state regulatory bodies, or organizations like The Joint Commission, which accredits many psychiatric hospitals.
Frequently Asked Questions about Psychiatric Hospitals
We understand that entering a psychiatric hospital can be a daunting experience, and many questions arise. Let’s address some common concerns to help explain the process.
What is a typical day like in a psychiatric hospital?
Life in a psychiatric hospital, or mental institution, is highly structured and focused on therapeutic activities. A typical day aims to provide a safe, predictable, and healing environment:
- Structured Daily Schedules: Days are planned with a clear routine, including wake-up times, meals, and scheduled activities.
- Group Therapy Sessions: These are a cornerstone of inpatient treatment, where patients share experiences, learn coping skills, and receive support from peers and therapists.
- Individual Counseling: Patients meet regularly with a therapist for one-on-one sessions to address specific issues and develop personalized treatment strategies.
- Medication Administration: Psychiatric medications are administered by nurses at scheduled times, with close monitoring for effectiveness and side effects.
- Recreational and Occupational Therapy: Activities like art therapy, music therapy, exercise, and life skills training are integrated to promote emotional expression, physical well-being, and practical skills.
- Mealtimes and Free Time: Meals are supervised, and there are designated periods for personal reflection, reading, or quiet activities. Staff checks are frequent to ensure safety.
The structured environment helps patients regain a sense of routine and stability, which is often crucial for recovery.
How long do people usually stay?
The length of stay in a psychiatric hospital varies significantly depending on the individual’s diagnosis, the severity of their symptoms, and their progress in treatment:
- Crisis Stabilization Units (CSUs): As mentioned, these are for very short-term, acute stabilization, typically lasting a few days (24-72 hours).
- Acute Inpatient Care: Stays in general inpatient psychiatric hospitals are usually short, often ranging from 1 to 2 weeks. The focus is on stabilizing acute symptoms and developing a discharge plan for ongoing care.
- Long-Term Residential Treatment: For severe and persistent mental illness, residential programs can involve stays of several months or even longer, providing comprehensive support and skill-building for community reintegration.
Discharge planning begins from day one, ensuring a smooth transition to the next appropriate level of care, whether it’s a partial hospitalization program, intensive outpatient program, or regular outpatient therapy. The average length of stay for an adult in a psych ward in the U.S. is around 5 to 7 days, based on 2018 data.
Can I have visitors or use my phone?
Policies regarding visitors and phone use can vary significantly between facilities, but they are always designed to balance patient privacy, connection with loved ones, and the overall safety and therapeutic environment:
- Designated Visiting Hours: Most facilities have specific visiting hours and may limit the number of visitors or require them to be on an approved list. This helps maintain structure and protects patient privacy.
- Rules on Phone and Internet Access: Access to personal phones and the internet is often restricted or supervised to prevent self-harm, maintain confidentiality, and ensure patients focus on their treatment. Some facilities may provide supervised phone time or computers for communication.
- Balancing Patient Privacy and Connection: The goal is to facilitate healthy connections while minimizing distractions and potential negative influences.
- Safety Protocols: These rules are also in place for safety. For example, items like shoelaces, belts, and certain electronics may be restricted to prevent self-harm. Visitors might also be searched to ensure no prohibited items enter the facility.
It’s always best to check with the specific facility regarding their policies before planning a visit or bringing personal items.
Conclusion: Finding the Right Path to Recovery
Psychiatric hospitals, or mental institutions, have undergone a profound change. They are no longer the places of isolation and despair depicted in historical narratives but have evolved into vital components of the modern mental healthcare system. Today, these facilities offer structured, evidence-based treatment designed to stabilize acute crises, manage complex conditions, and equip individuals with the skills needed for recovery and reintegration into their communities.
The journey from the “asylum” model to recovery-focused care reflects a deeper understanding of mental illness—recognizing it as a treatable health condition rather than a moral failing. Hope and recovery are not just possibilities; they are the driving principles behind contemporary psychiatric treatment.
We understand that seeking help for mental health challenges can be daunting, and the stigma associated with psychiatric care can still be a barrier. However, it’s crucial to remember that you are not alone, and reaching out is a courageous first step towards healing. Whether it’s a brief stay in a crisis stabilization unit, an intensive inpatient program, or long-term residential care, the right support can make all the difference.
At SoberSteps, we provide a confidential and anonymous platform to help you steer the complexities of mental health and substance use disorder treatment. We are here to connect you with the resources and care you need, offering a guiding hand on your path to recovery. Don’t wait to take that crucial first step. If you or someone you love needs help, please call us today at (844) 491-5566. Your journey to healing begins now.