Why Understanding Mental Health Crises Matters Now More Than Ever
A mental health crisis is a situation where an individual experiences acute distress that overwhelms their ability to cope, potentially leading to harm to themselves or others. If you or someone you know is in immediate danger:
- Call 911 if there is imminent risk of harm
- Text or call 988 to reach the Suicide & Crisis Lifeline (available 24/7)
- Go to the nearest emergency room for immediate psychiatric evaluation
- Call (844) 491-5566 for confidential crisis support and treatment referrals
The numbers paint a sobering picture. In the United States alone, an estimated 59.3 million adults—nearly 1 in 4—experienced a mental illness in 2022. Of these, 15.4 million faced serious mental illness that substantially interfered with major life activities. Globally, more than a billion people live with a mental health condition, and suicide claimed an estimated 727,000 lives in 2021.
This isn’t just a personal struggle. It’s a public health emergency that affects families, communities, and entire societies. The global economy loses an estimated $1 trillion each year in lost productivity due to depression and anxiety alone.
A mental health crisis differs from everyday stress or ongoing mental health challenges. It represents an acute breaking point—when someone can no longer function safely, when thoughts of suicide emerge, or when behavior becomes dangerous. Understanding this distinction can save lives.
This guide will help you recognize the warning signs of a mental health emergency, know exactly what steps to take when crisis strikes, and understand the broader support systems available. Whether you’re seeking help for yourself or supporting someone else, you’ll find clear, actionable information to steer these critical moments.
At Sober Steps, we’ve dedicated ourselves to providing confidential, anonymous support for individuals navigating mental health crises and substance use disorders, connecting thousands with the treatment resources they need to begin recovery. Our mission is to ensure no one faces these challenges alone.
Recognizing the Warning Signs of a Mental Health Emergency
Recognizing the warning signs of a mental health crisis is the first critical step toward getting help. These signs can manifest in various ways, affecting a person’s thoughts, emotions, and behaviors. It’s important to distinguish between a “bad day” and a true crisis, where an individual’s safety or the safety of others may be at risk.
Behavioral Signs
Behavioral changes are often the most noticeable indicators that someone is struggling. These might include:
- Social Withdrawal: Isolating from friends, family, and activities they once enjoyed.
- Neglecting Self-Care: A sudden disregard for personal hygiene, maintaining their living space, or eating regularly.
- Increased Substance Use: Relying more heavily on alcohol, drugs, or prescription medications to cope.
- Risky or Impulsive Behaviors: Engaging in uncharacteristic, reckless, or dangerous activities like excessive spending or driving under the influence.
- Changes in Sleep Patterns: Sleeping much more or less than usual, or severe insomnia.
- Changes in Appetite: Significant weight loss or gain.
Emotional Signs
Emotional indicators dig deeper into the person’s internal experience. While these can be harder to spot, they are crucial:
- Extreme Mood Swings: Rapid, dramatic shifts in mood, from intense happiness to deep despair or irritability.
- Intense Anxiety or Paranoia: Overwhelming feelings of worry or fear, sometimes with irrational suspicions.
- Hopelessness or Despair: A pervasive sense that things will never get better or a feeling of being trapped.
- Agitation or Restlessness: An inability to sit still, constant pacing, or feeling on edge.
- Overwhelming Guilt or Shame: Persistent feelings of worthlessness or excessive self-blame.
Verbal Cues
What someone says can directly signal a mental health crisis, especially regarding suicidal ideation. Pay close attention to:
- Talking about Suicide or Self-Harm: Direct statements like “I want to die” or indirect ones like “I can’t take this anymore.”
- Expressing No Reason to Live: Statements indicating a lack of purpose in life.
- Feeling Like a Burden: Believing others would be better off without them.
- Saying Goodbye: Giving away possessions or saying farewell in an unusual manner.
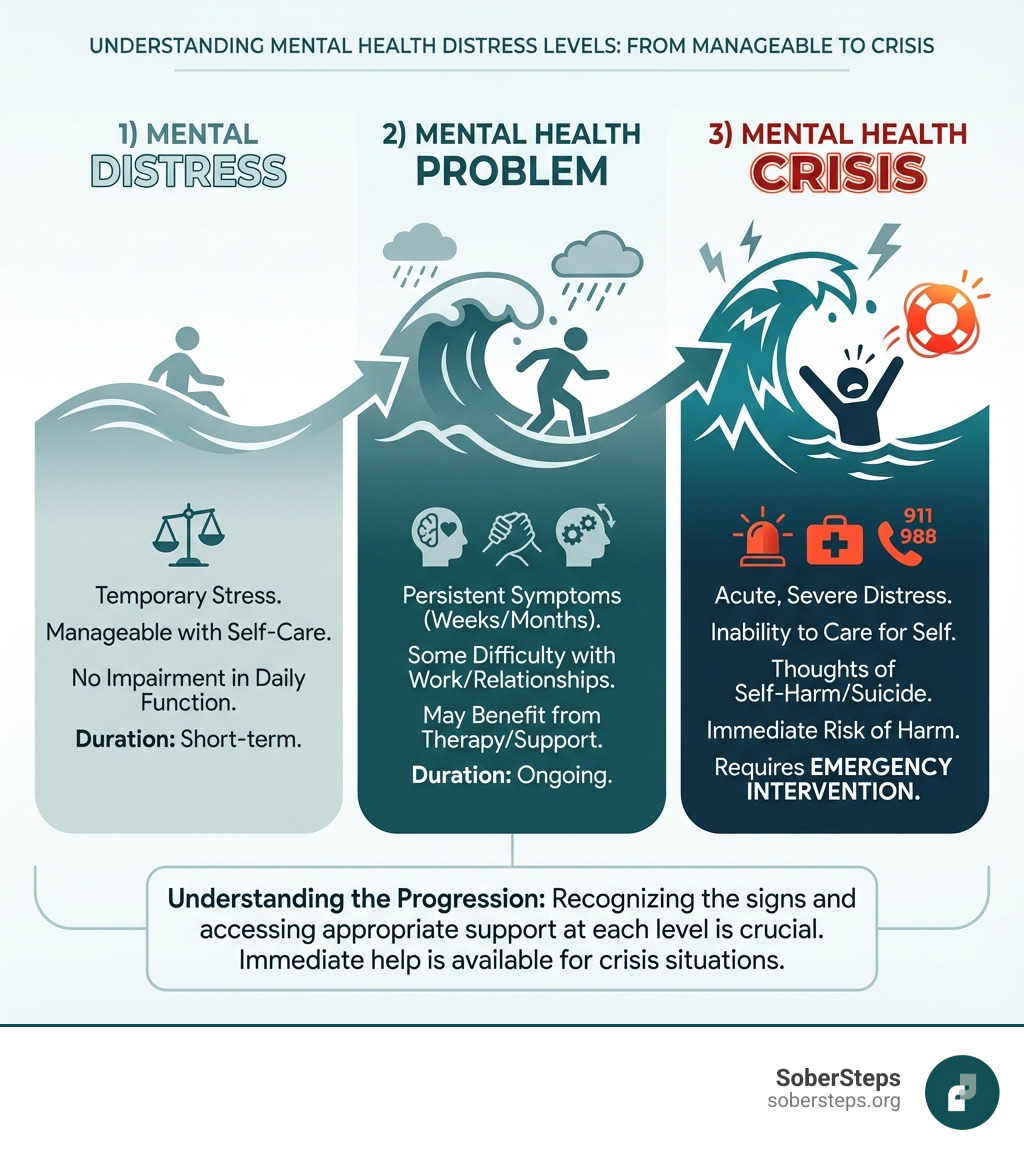
Crisis vs. Non-Crisis: Understanding the Difference
It’s important to understand the distinction between a mental health crisis and a non-crisis mental health need.
- A mental health crisis involves acute distress and a clear risk of harm to oneself or others. This includes active suicidal thoughts, severe psychosis, or extreme agitation. These situations require immediate intervention.
- A non-crisis mental health need refers to ongoing challenges like chronic depression or anxiety that are not immediately life-threatening. While serious, these needs allow for planned, long-term support, as the individual can generally maintain their safety.
If you observe these warning signs, particularly a combination of them, it’s crucial to take them seriously and act promptly.
Immediate Steps to Take in a Crisis: A Lifeline When You Need It Most
When someone is experiencing a mental health crisis, immediate action can make all the difference. The priority is to ensure safety and connect the individual with appropriate care. Here are the immediate steps you should take:
-
Assess for Immediate Danger: First, determine if there is an imminent threat of harm to the individual or others. Are they attempting self-harm, threatening violence, or in immediate physical danger?
- If harm is imminent, call 911 immediately. Emergency services can provide urgent intervention and transport to a hospital for situations threatening life or safety.
-
For Suicidal Thoughts or Concerns: If you or someone you know is experiencing suicidal thoughts, there are dedicated resources for immediate support:
- Call or text 988 to reach the 988 Suicide & Crisis Lifeline. This national service is available 24/7, offering free, confidential support. You can reach them at 988 Suicide & Crisis Lifeline.
- Go to the nearest hospital emergency room. An ER is equipped to handle mental health emergencies, providing a safe environment, assessment, and connection to psychiatric services.
-
Contact a Crisis Hotline: Beyond 988, various hotlines offer immediate, confidential support and referrals.
- For confidential crisis support and treatment referrals, call our helpline at (844) 491-5566. We are here to help you steer these challenging moments.
- The SAMHSA National Helpline at 1-800-662-HELP (4357) offers 24/7 treatment referral and information.
- The Disaster Distress Helpline at 1-800-985-5990 provides 24/7 crisis counseling for emotional distress following any traumatic event.
-
Remove Access to Means of Self-Harm: If someone is suicidal, it’s crucial to remove potential means of self-harm from their environment (e.g., firearms, medications, sharp objects). This simple step can create a vital window for intervention.
Taking these immediate steps can stabilize a mental health crisis and ensure the individual gets the professional help they need. You don’t have to face this alone.
Navigating the Broader Mental Health Crisis and Support Systems
Addressing a mental health crisis requires understanding the diverse landscape of available support systems. From immediate intervention to ongoing care, these services play distinct but interconnected roles in recovery.

Community vs. Hospital Care
What’s the difference between community-based and hospital-based services, and when is each appropriate?
- Role of Community-Based Services: These services (e.g., walk-in crisis centers, mobile crisis teams) provide support in less restrictive environments. They focus on de-escalation, safety planning, and connecting individuals to resources, aiming to avoid hospitalization when possible.
- When Hospital Care is Necessary: Hospital care is for a mental health crisis that poses a severe risk that cannot be managed in the community, such as active suicidal intent or psychosis. Hospitals provide intensive, 24/7 care and a secure environment for stabilization.
Types of Crisis Services
A range of services exists to meet different crisis needs:
- Crisis Hotlines and Warmlines: Services like 988 offer immediate emotional support, de-escalation, and referrals via phone or text. Warmlines provide peer support for non-crisis situations.
- Mobile Crisis Teams: These teams of mental health professionals respond to individuals in crisis in their homes or communities, providing on-site assessment and de-escalation.
- Walk-in Crisis Centers: These centers offer immediate, face-to-face support without an appointment.
- SoberSteps Crisis Support and Referral Services: We offer confidential and anonymous access to information and referrals for mental health and substance use disorders. Our helpline at (844) 491-5566 is a direct line to help you find the right support.
- Telehealth and Digital Resources: Virtual counseling and mental health apps have significantly expanded access to crisis intervention, especially for those in rural or underserved areas.
Systemic Challenges
Despite these services, our mental health crisis care systems face significant challenges:
- Gaps in Care: Many areas lack integrated crisis care, creating a disconnect between emergency, community, and long-term services.
- Workforce Shortages: A critical shortage of mental health professionals leads to long wait times, fewer crisis responders, and staff burnout.
- Stigma as a Barrier: Stigma often prevents people from seeking help until a crisis occurs due to fear of judgment. Our commitment at Sober Steps is to provide a confidential and anonymous platform to help overcome this barrier.
The Growing Scale of the Mental Health Crisis
The United States is experiencing a profound mental health crisis, impacting individuals across all demographics. Understanding its scope is crucial for effective intervention.
U.S. Statistics
The data reveals a stark reality:
- In 2022, an estimated 59.3 million adults aged 18 or older in the United States had Any Mental Illness (AMI), representing 23.1% of all U.S. adults. AMI is a mental, behavioral, or emotional disorder with varying levels of impairment.
- Of these, 15.4 million adults had Serious Mental Illness (SMI), or 6.0% of all U.S. adults. SMI results in serious functional impairment that interferes with major life activities.
- Alarmingly, only 50.6% of adults with AMI received mental health treatment in the past year. While treatment rates for SMI were higher at 66.7%, a significant portion still goes untreated.
- You can explore more detailed statistics at Mental Health By the Numbers.
Global Perspective
This is part of a larger global issue. More than a billion people worldwide live with a mental health condition. The global economy loses an estimated $1 trillion each year in lost productivity due to issues like anxiety and depression, underscoring the urgency of addressing the mental health crisis at every level.
Youth Mental Health
One of the most concerning aspects of the crisis is its impact on young people:
- An estimated 49.5% of adolescents aged 13-18 in the U.S. had any mental disorder in their lifetime, meaning nearly half experience a diagnosable condition before adulthood.
- The CDC confirms the U.S. is in a mental health crisis, especially among young people. This trend has been worsened by the pandemic, with drug overdose and suicide remaining leading causes of death.
The sheer scale of these numbers highlights that mental health challenges are a widespread public health emergency.
Specialized Support for Diverse Populations
A mental health crisis can affect anyone, but certain populations face unique challenges. At Sober Steps, we help individuals from all walks of life find the resources they need.
- Youth and Young Adults: Many conditions first emerge during these critical years. Youth resources focus on early intervention and peer support. SoberSteps helps locate youth-specific programs. Call us at (844) 491-5566 to find support.
- Veterans: Service members often face PTSD, depression, and anxiety. Specialized programs offer trauma-informed care and peer support. SoberSteps connects veterans with providers who understand their unique experiences. Call us at (844) 491-5566 to find support.
- Seniors: Older adults face issues like depression and anxiety, often linked to loneliness or chronic illness. Support focuses on social connection and age-appropriate care. SoberSteps helps seniors find accessible care options. Call us at (844) 491-5566 to find support.
- BIPOC Communities: These communities face disproportionate rates of mental illness and barriers to care. Culturally competent care is essential. SoberSteps helps connect individuals with inclusive providers. Call us at (844) 491-5566 to find support.
- Rural and Underserved Areas: Residents often face limited access to mental health services. Telehealth options have become a critical lifeline, and local public health resources help bridge these gaps. Our platform can help find available telehealth providers and local support networks. Call us at (844) 491-5566 to find support.
By addressing the specific needs of these diverse populations, we can work towards a more equitable and effective mental health support system.
How to Support a Loved One and Find Help After the Storm
A Guide for Family, Friends, and Survivors of the Mental Health Crisis
Supporting someone through a mental health crisis is challenging, but your informed actions are invaluable. If you’re a family member, friend, or a survivor of suicide loss, here’s how we can help:
-
How to Help:
- Listen Without Judgment: Offer a safe, non-critical space for them to express their feelings. Validate their emotions by saying, “That sounds incredibly difficult.”
- Offer Practical Support: Help with overwhelming daily tasks like making appointments, preparing meals, or running errands.
- Encourage Professional Help: Gently suggest seeking professional support. Offer to help them find a therapist or accompany them to an appointment. Remind them that seeking help is a sign of strength.
-
Creating a Safety Plan: If your loved one is at risk of self-harm, collaborating on a crisis plan is essential. The plan should outline warning signs, coping strategies, support contacts (friends, family, professionals), emergency numbers like 988, and steps to remove means of self-harm.
-
Coping with Suicide Loss: For those who have lost a loved one to suicide, the grief is often complex. You are not alone, and support is available:
- Support for Survivors: Seek out survivor support groups or counseling for suicide loss. These resources provide a safe space to process grief and reduce isolation. Online resources can also be helpful.
- The SAMHSA Disaster Distress Helpline (1-800-985-5990) can offer immediate counseling for emotional distress related to traumatic loss.
-
Self-Care for Caregivers: Supporting someone in a mental health crisis can take a toll on your own well-being. Prioritize your self-care to avoid burnout:
- Set boundaries and know your limits.
- Seek your own support from a friend, family member, or therapist.
- Make time for hobbies, exercise, or relaxation.
- Taking care of yourself allows you to be a more effective source of support.
Finding Ongoing Treatment and Preparing for the Future
A mental health crisis is often a turning point. Once the immediate danger has passed, the journey toward long-term recovery begins.
- Transitioning from Crisis Care: The next steps involve transitioning from emergency support to ongoing treatment, such as moving from a hospital to an outpatient program or from a crisis hotline to regular therapy.
- Finding Long-Term Support: Sustained recovery requires consistent support.
- Locating Therapists: Finding a good therapist is crucial. Use online directories, get referrals, or use platforms like SAMHSA’s FindTreatment.gov.
- Support Groups: Peer support groups like those offered by the National Alliance on Mental Illness (NAMI) provide community and shared experience.
- SoberSteps Treatment and Recovery Programs: At Sober Steps, we connect individuals with a broad network of treatment and recovery programs. Our confidential platform makes it easier to find the right long-term support. Call us at (844) 491-5566 to explore your options.
- Building Resilience: Beyond formal treatment, building personal resilience is key. This involves developing coping strategies, practicing mindfulness, staying physically active, and fostering strong social connections.
Frequently Asked Questions about Mental Health Emergencies
What is the difference between a bad mental health day and a mental health crisis?
A “bad mental health day” involves manageable feelings of sadness or stress, where you can still function and remain safe. A mental health crisis is an acute situation where your ability to cope is overwhelmed. It involves intense distress, severe functional impairment, or an immediate risk of harm to yourself or others (like active suicidal thoughts). A crisis requires immediate intervention to ensure safety.
Can I force someone to get help during a crisis?
Involuntary commitment laws vary by state but generally apply if a person is an immediate danger to themselves or others, or is gravely disabled. This legal process is initiated by professionals or law enforcement after an assessment. If you believe someone meets this criteria, contact 911 or a crisis team; you cannot force them into treatment yourself.
What is the 988 Lifeline and when should I use it?
The 988 Suicide & Crisis Lifeline is a national, 24/7, free, and confidential service. You should call or text 988 if you or someone you know is experiencing:
- Suicidal thoughts or feelings.
- A mental health crisis or emotional distress.
- A substance use crisis.
- Worry about a loved one who might be in crisis.
It connects you with trained crisis counselors who provide immediate support, de-escalation, and connections to local resources.
Conclusion
This guide has covered how to recognize the signs of a mental health crisis, what immediate steps to take, and how to steer the landscape of support systems. We’ve also highlighted the importance of ongoing treatment and the critical role loved ones play in recovery.
The numbers are clear: the mental health crisis is a pervasive challenge. But amidst these statistics, there is a powerful message of hope. Recovery is a reality for countless individuals who receive timely and appropriate support. Help is available, and no one has to steer these challenges alone.
At Sober Steps, our commitment is unwavering. We strive to be a guide of hope, providing confidential and anonymous access to mental health and substance use treatment resources. We believe that by fostering understanding and connecting individuals to the right care, we can collectively move beyond the brink.
If you or a loved one is struggling, don’t wait. Call us at (844) 491-5566 or explore our specialized treatment options to find the confidential support you deserve.