Best Drug Rehabs Sevier County TN 2026
Explore the best drug rehab Sevier County TN centers. Find comprehensive addiction treatment, financial aid, and local support. Call for help.
Highmark is one of America’s largest Blue Cross Blue Shield-affiliated health insurers, serving approximately 7 million members across Pennsylvania, West Virginia, Delaware, and parts of New York. If you’re struggling with substance use disorder and have Highmark insurance, understanding your coverage is the first step toward recovery.
Quick Answer: Does Highmark Cover Addiction Treatment?
| Treatment Type | Usually Covered | What to Know |
|---|---|---|
| Medical Detox | Yes | May require pre-authorization |
| Inpatient Rehab | Yes | Duration limits may apply |
| Outpatient Programs (PHP/IOP) | Yes | Often preferred by insurers |
| Individual Therapy | Yes | Part of essential health benefits |
| Medication-Assisted Treatment | Yes | Includes Suboxone and Methadone |
Drug and alcohol addiction is a serious condition, but financial concerns shouldn’t block your path to recovery. Health insurance plans like Highmark are required by the ACA to cover treatment for substance use disorders as an essential health benefit.
Your Highmark plan likely covers multiple levels of care, from inpatient treatment to outpatient support. Specifics depend on your plan type (HMO, PPO, etc.) and tier (Bronze, Silver, Gold), but the core coverage is there.
You don’t have to steer this alone. At Sober Steps, we specialize in helping people understand their Highmark coverage and find the right treatment. We can guide you through the insurance verification process to help you access the care you need.
For immediate, confidential assistance with your Highmark benefits, call (844) 491-5566 anytime, day or night.
Highmark is a major nonprofit healthcare company and integrated delivery network based in Pittsburgh, Pennsylvania. It’s a comprehensive organization that blends health insurance with healthcare delivery. As an independent licensee of the Blue Cross Blue Shield Association, Highmark operates under the trusted Blue Cross and Blue Shield brand.
Our research shows that Highmark’s geographic reach primarily spans the Northeast and Mid-Atlantic United States, serving members in:
This broad footprint allows Highmark to serve a diverse population. Highmark, the US healthcare provider, is distinct from “HiMark,” a Canadian company in a different industry. Our focus here is solely on the US healthcare provider, Highmark.

As an integrated delivery network, Highmark combines insurance plans with direct healthcare services, notably through its Allegheny Health Network. Its mission is “to create a remarkable health experience, freeing people to be their best.” The organization provides a wide array of services, including:
Highmark also actively engages in community initiatives, demonstrating a commitment to social responsibility alongside its core business.
Highmark uses technology to improve the member experience. The My Highmark App is a one-stop solution for members to manage their plan, find doctors, and pay bills from their smartphone.
Beyond administrative tools, the company offers virtual care options like Virtual Joint Health, Thrive by Sword², a virtual physical therapy service for at-home recovery. Other innovations, like the EQ Active brain function assessment platform, align with Highmark’s goal of proactive, integrated health management. Highmark also provides online tools, such as their interactive quiz: Find the Best Plan for You. These tools underscore Highmark’s commitment to creating a more responsive and empowering healthcare experience.

Understanding your Highmark coverage for addiction treatment is a critical first step. Federal laws like the Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act (MHPAEA) mandate that most plans cover substance use disorder services.
This ensures your plan covers medically necessary care, meaning a doctor-approved treatment plan will guide the process. The MHPAEA also ensures that cost-sharing for addiction treatment is no more restrictive than for medical care, which is vital for treating co-occurring disorders.
Your costs are heavily influenced by using in-network vs. out-of-network providers. In-network facilities offer the lowest costs, while out-of-network care, if covered, will lead to higher deductibles and coinsurance.
Verifying your benefits is the best way to avoid surprises. Call our confidential helpline at (844) 491-5566 for a free insurance check. We can help you understand your Highmark plan and find suitable treatment.
Highmark insurance plans typically cover a comprehensive range of addiction treatment services. The specific types of treatment covered may include:
The specific extent of coverage for each of these services will depend on your individual Highmark plan. Always verify your benefits to understand your personal coverage details.
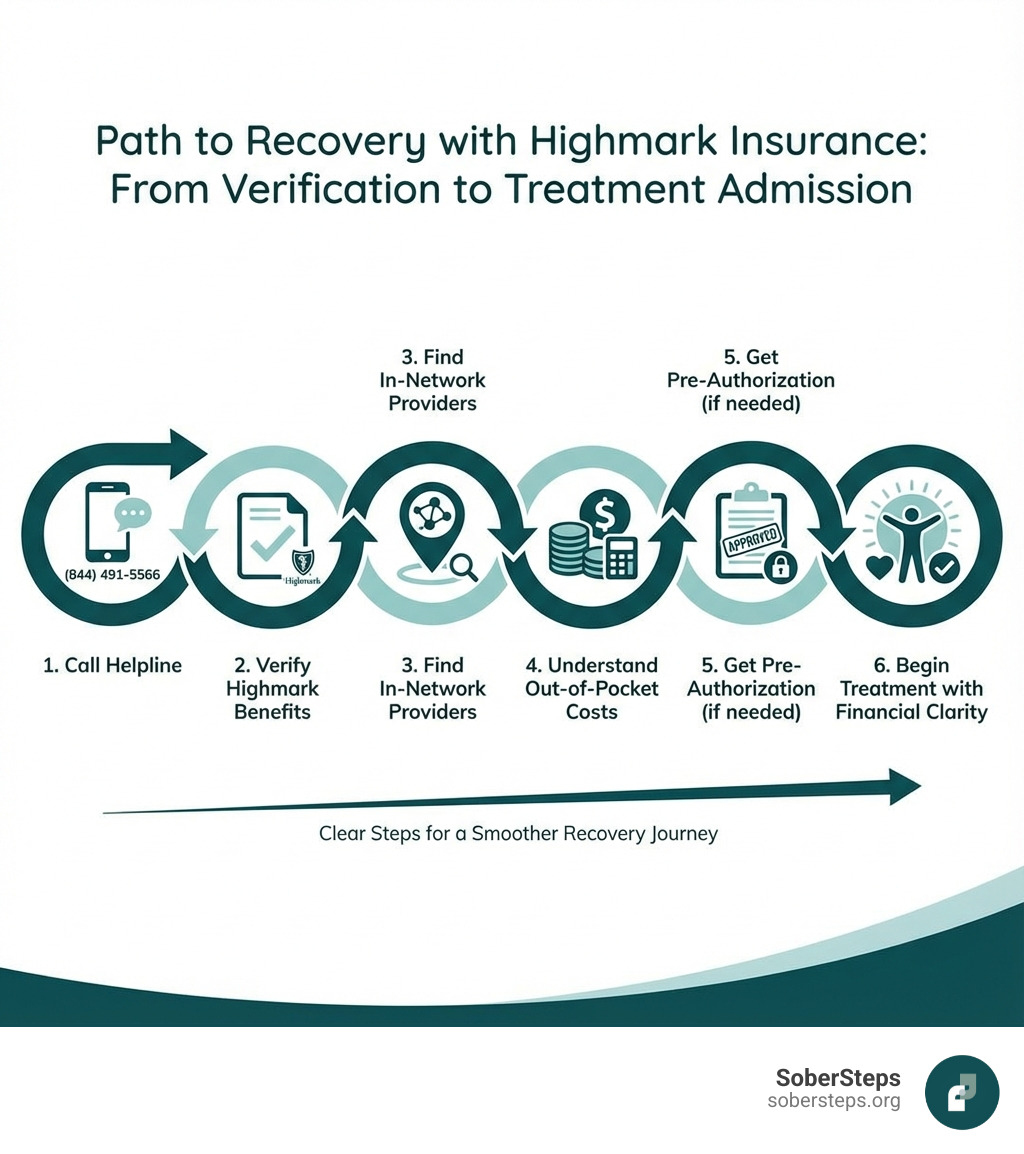
Verifying your Highmark insurance coverage for rehab is a crucial step before beginning treatment. Here’s how you can do it:
By taking these steps, you can ensure you have a clear picture of your Highmark rehab coverage, allowing you to focus on what truly matters: your recovery.
Highmark offers a variety of health insurance plans to meet diverse needs. These plans fall into several main categories:
Beyond these categories, Highmark plans are structured using different managed care models:
Understanding these plan types is key to knowing how your Highmark coverage will work for addiction treatment.
Highmark also categorizes its ACA marketplace plans by “metallic levels,” which indicate how you and your plan share costs.
When considering any Highmark plan, understand these key out-of-pocket costs:
Choosing the right plan involves balancing monthly premiums with potential out-of-pocket expenses. If you need help finding affordable care options with your Highmark plan, call us at (844) 491-5566 to discuss your options.
For seniors, Highmark offers Medicare plans that cover addiction and mental health. You can Learn about Medicare on their site. Options include:
Verifying your specific Medicare plan benefits is crucial to understand your coverage for addiction treatment.
Understanding health insurance can be complex. Here, we address some of the most common questions about Highmark coverage for addiction treatment.
Yes, Highmark plans cover mental health services like therapy. The Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act (MHPAEA) mandate that mental health and substance use disorder services are covered as essential health benefits, with parity to medical benefits. This means your plan typically covers:
Always check your specific Highmark plan for details on copayments, deductibles, and network restrictions.
This depends on your plan type. This is a common question, and the answer varies.
Crucially, you must verify your out-of-state benefits with Highmark before choosing a facility. Ask about out-of-network coverage, costs, and any pre-authorization requirements.
A denial is not the final word. You have the right to appeal Highmark’s decision.
Work with your healthcare providers to ensure they submit comprehensive medical necessity documentation. If appeals fail or you need immediate help, explore alternative financing like payment plans from treatment centers, sliding scale fees, grants, or healthcare loans. Don’t give up if your initial request is denied; persistent advocacy can often lead to a successful outcome. If you need help navigating an appeal, call our confidential helpline at (844) 491-5566.
The key takeaway is that your Highmark insurance plan likely provides significant coverage for addiction treatment. Federal laws ensure that services like detox, inpatient rehab, outpatient programs, and therapy are covered benefits.
However, understanding the specifics of your plan (HMO, PPO, etc.) and its costs is crucial for making informed decisions. Navigating these details can be stressful, but you don’t have to do it alone. Verifying your benefits is the most important step, as it provides the clarity needed to focus on your recovery.
At Sober Steps, we are here to help you understand your options and connect you with the right care. Take the first step toward a healthier life by learning more about using your insurance for treatment. For immediate and confidential support, call our 24/7 helpline at (844) 491-5566. Your journey to recovery can start now.
Explore the best drug rehab Sevier County TN centers. Find comprehensive addiction treatment, financial aid, and local support. Call for help.

Conquer cravings in recovery! Get help with cravings using science-backed strategies, mindfulness, and professional support for lasting sobriety.
Understand modern mental institution care, types, and how to access help for recovery. Call (844) 491-5566 for support.
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.