Understanding Rapid Detox: What You Need to Know Before Deciding
Rapid detox centers offer a controversial approach to opioid withdrawal that promises to eliminate the worst symptoms in just a few days. Here’s what you need to know:
Key Facts About Rapid Detox:
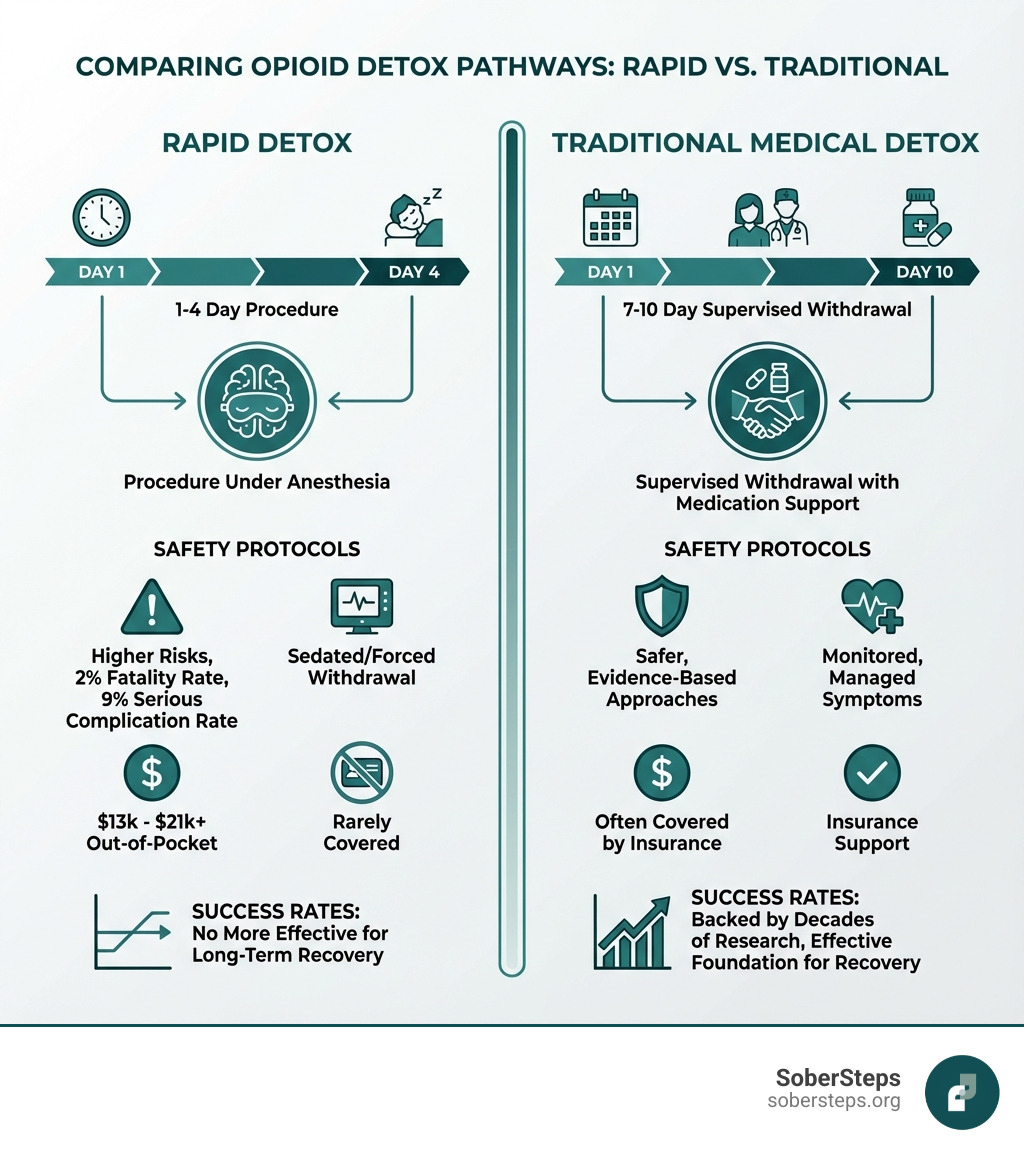
- What it is: A procedure where patients are sedated or put under anesthesia while doctors administer opioid-blocking drugs to force withdrawal
- Duration: Typically 1-4 days, compared to 7-10 days for traditional medical detox
- Cost: $13,000-$21,000+ out of pocket (insurance rarely covers it)
- Safety concerns: CDC study found a 2% fatality rate and 9% serious complication rate
- Effectiveness: Studies show it’s no more effective than traditional detox for long-term recovery
- Best for: Only opioid addiction (heroin, fentanyl, prescription painkillers)
- Not for: Alcohol, benzodiazepines, or stimulants
The Bottom Line: While rapid detox sounds appealing, research indicates it carries significant risks without proven advantages over safer, evidence-based medical detox approaches.
If you’re struggling with opioid dependence, the promise of sleeping through withdrawal and waking up “cured” can sound like a miracle. But is it too good to be true? The answer requires looking beyond the marketing claims.
Traditional medical detox takes longer and requires conscious management of withdrawal symptoms. But it’s also safer, often covered by insurance, and backed by decades of research. Rapid detox, by contrast, remains experimental—and potentially dangerous.
At Sober Steps, we’re committed to helping individuals and families steer addiction treatment with honest, research-backed information. Our team has extensively reviewed rapid detox centers and alternative treatment approaches to help you understand what’s safe, what’s effective, and what questions to ask before making this critical decision.
Learn more about finding quality addiction treatment
The Allure of a Quick Fix
When facing the daunting prospect of opioid withdrawal, the idea of a “fast track to freedom” can be incredibly enticing. Opioid dependence can create a powerful physical and psychological grip, and the thought of enduring days or weeks of intense discomfort—nausea, vomiting, muscle cramps, anxiety, and profound fatigue—is enough to make anyone seek an alternative. This is where the allure of rapid detox centers comes in.
These programs often promise a painless detox, where you can literally sleep through the worst of withdrawal, emerging hours or a few days later with the physical dependence seemingly behind you. It sounds like a shortcut, a way to bypass the suffering and get straight to recovery. For someone struggling with Opioid Use Disorder, this can feel like the answer to a desperate prayer. However, as we’ll explore, this quick fix often comes with significant risks and doesn’t address the full scope of addiction.
How It Differs from Standard Medical Detox
The fundamental difference between rapid detox and traditional medical detox lies in the speed and method of withdrawal induction.
In traditional medical detox, patients undergo a supervised withdrawal process, typically lasting 7 to 10 days or more, depending on the substance and individual needs. This method focuses on managing withdrawal symptoms with medications in a conscious state, ensuring comfort and safety. The body gradually rids itself of opioids, and healthcare professionals monitor vital signs and administer medications to ease discomfort. This approach prioritizes patient stability and continuous medical oversight. For a deeper understanding of the different levels of care, including detox, you can explore our resources on More info about detox levels of care.
Rapid detox, also known as anesthesia-assisted rapid opioid detox (AAROD) or ultra-rapid opiate detox, takes a drastically different approach. Instead of gradual withdrawal, it aims to accelerate the process by inducing a rapid, or “precipitated,” withdrawal while the patient is under general anesthesia or deep sedation. The goal is for the patient to be unconscious during the most severe physical withdrawal symptoms. While the idea is to reduce the conscious experience of withdrawal, this intense acceleration of the body’s response carries a unique set of safety considerations that distinguish it sharply from standard medical detox protocols.
The Procedure: How Anesthesia-Assisted Detox Works
The Role of Anesthesia and Sedation

At the heart of rapid detox is the use of anesthesia or deep sedation. The primary purpose is to render the patient unconscious, preventing them from experiencing the often severe and immediate withdrawal symptoms that occur when opioid antagonists are introduced. This means that for a period, typically several hours, the patient is under general anesthesia, similar to what one might receive during surgery.
During this time, a qualified anesthesiologist closely monitors the patient’s vital signs, ensuring their safety while their body undergoes an intense physiological process. The idea is that by sleeping through withdrawal, patients avoid the physical and psychological trauma associated with traditional detox. However, while the patient may not be consciously aware of the symptoms, their body is still experiencing them, sometimes with alarming intensity, which can put significant stress on various organ systems.
Forcing Withdrawal with Opioid Antagonists
Once the patient is under anesthesia, the real “rapid” aspect of the detox begins. Medical professionals administer opioid antagonists, such as Naloxone or naltrexone. These medications work by blocking opioid receptors in the brain and body. When these receptors are blocked, any opioids present are displaced, and the body is forced into an immediate, accelerated withdrawal.
Think of it like this: your body’s opioid receptors are like keyholes, and opioids are the keys that fit perfectly, producing their effects. Opioid antagonists are like different keys that also fit the keyholes but don’t open the lock; instead, they block the original keys from getting in. This sudden blockage causes the body to react intensely, as it’s abruptly deprived of the opioids it has become dependent on. This forced removal of opioids from the body is what precipitates the rapid and often severe withdrawal symptoms. For those who experience persistent cravings even after detox, understanding options for Help with Cravings is crucial for long-term recovery.
What Substances Can Be Treated?
Rapid detox methods, particularly those involving opioid antagonists, are primarily designed for opioid addiction. This includes dependence on substances such as:
- Heroin
- Fentanyl (including illicit fentanyl, which can be particularly potent and dangerous to detox from)
- Prescription painkillers (e.g., oxycodone, hydrocodone, morphine, Percocet)
- Methadone (often used in medication-assisted treatment, but can also lead to dependence)
- Other opioids like Suboxone, Subutex, Dilaudid, Demerol, Kratom, and Tramadol.
The use of opioid antagonists specifically targets the opioid receptor system. Therefore, rapid detox is not effective or safe for other types of substance dependence, such as alcohol or benzodiazepines. Withdrawal from these substances requires different medical protocols and can be life-threatening if not managed appropriately with specific medications. If you are struggling with opioid addiction, seek treatment custom to your specific needs.
The High Stakes: Unpacking the Risks and Controversies of Rapid Detox Centers
Significant Health Dangers and Life-Threatening Complications

While the promise of a painless, quick detox is appealing, the reality of rapid detox can be fraught with danger. The accelerated, forced withdrawal under anesthesia places immense stress on the body, leading to a range of severe and potentially life-threatening complications. Our research shows that adverse side effects of rapid or ultra-rapid detox can include:
- Severe vomiting or diarrhea: This can lead to rapid dehydration and electrolyte imbalances, which can be critical.
- Low blood pressure: A sudden drop in blood pressure can deprive organs of necessary blood flow.
- Delirium: A state of acute confusion and altered consciousness.
- Aspiration pneumonia: If a patient vomits while under anesthesia or in a deeply sedated state, they can inhale stomach contents into their lungs, leading to a severe lung infection.
- Pulmonary edema: A buildup of fluid in the lungs, making breathing difficult.
- Diabetic ketoacidosis: A serious complication of diabetes that can occur when the body produces high levels of blood acids called ketones.
- Sudden death: Tragically, this is a documented risk.
A study highlighted by the Centers for Disease Control and Prevention (CDC) found alarming statistics: out of 75 people who underwent rapid detox, two died and five had serious health effects. This equates to a more than 2% fatality rate and a 9% rate of serious complications. Given that medically assisted detox almost never results in death or serious complications, these figures raise significant concerns. You can read more about these findings in the CDC report on severe adverse events.
Furthermore, it’s a common misconception that rapid detox eliminates all withdrawal symptoms. While the patient is unconscious during the initial, most acute phase, many people are surprised to learn that withdrawal symptoms can still be expected after rapid detox. These often include psychological symptoms like cravings, anxiety, and depression, as well as physical discomforts like irritability, yawning, and goosebumps. A study comparing withdrawal symptoms notes that symptoms like restlessness can persist. For more details, refer to the Study on post-detox symptoms.
Ethical Concerns and Lack of Regulation
The significant risks associated with rapid detox procedures have led to considerable ethical debate and controversy within the medical and addiction treatment communities. Many healthcare professionals consider it an experimental form of treatment, prioritizing comfort over proven safety and long-term effectiveness.
The intensive nature of rapid detox procedures demands exceptional medical expertise and facility standards. Ideally, such a procedure should be performed in a fully accredited hospital setting, specifically within a private ICU room, with continuous monitoring by board-certified physicians, including an anesthesiologist, and a highly trained medical team. This level of care is essential to manage the potential for severe complications. However, not all rapid detox centers operate with these rigorous standards, leading to concerns about patient safety being compromised for profit.
The lack of consistent regulation and the experimental classification mean that individuals seeking this treatment need to be incredibly vigilant. We believe that choosing safe and effective addiction treatment means prioritizing evidence-based care and transparency. Find safe and effective addiction treatment that adheres to the highest medical standards.
Who Is a Good Candidate and Who Must Avoid It?
Given the inherent risks, rapid detox is certainly not for everyone. A thorough pre-screening and medical evaluation are absolutely essential to determine if a patient can even safely undergo the procedure.
Individuals who are generally considered high-risk and should avoid rapid detox include those with:
- Pre-existing heart conditions
- Lung diseases
- Significant metabolic issues (like uncontrolled diabetes)
- Severe mental health disorders
- A history of seizures
- Any other serious medical conditions that could be exacerbated by the stress of rapid, induced withdrawal and anesthesia.
Discussing all potential risks and your full medical history with a qualified doctor is paramount. It’s not just about getting off opioids quickly; it’s about doing so in a way that preserves your health and sets you up for successful, long-term recovery. Don’t hesitate to ask detailed questions about the medical team, the facility’s accreditation, and emergency protocols.
Effectiveness and Cost: Is It a Worthwhile Investment?
Long-Term Success and High Relapse Rates
One of the most critical questions surrounding rapid detox is its effectiveness for long-term addiction recovery. While it may offer a quick way to clear opioids from the body, research does not show that rapid detox is any more effective than traditional detox methods for sustained sobriety. In fact, it may even be worse in terms of long-term success.
Detoxification, regardless of the method, is only the very first step in addressing addiction. It clears the physical dependence, but it does not treat the underlying psychological components of addiction—the cravings, triggers, coping mechanisms, and behavioral patterns that lead to substance use.
Studies indicate that when rapid opioid detox is used alone, it has a very high rate of relapse. This is partly because patients experience little to no discomfort during the detox, which might reduce their incentive to avoid future opioid use. More importantly, without follow-up care that addresses the psychological roots of addiction, individuals are highly vulnerable to returning to substance use. We cannot stress enough that detox itself does little to actually help someone maintain sobriety long-term. To truly build a life in recovery, ongoing therapy, counseling, and support are indispensable. Learn more about Learn about relapse prevention strategies.
The Financial Burden of Rapid Detox
Beyond the questions of safety and long-term effectiveness, there’s the significant financial aspect to consider. Rapid detox is generally quite expensive, and the cost can be a major barrier for many individuals and families.
People who choose to undergo rapid detox should expect to pay anywhere from $13,000-$15,000 out of pocket, though costs will vary depending on the individual facility. Some well-established providers may charge significantly more, with prices upwards of $21,000 or even $28,000 for extended stays.
Adding to this financial burden is the fact that many major health insurance companies will not pay for it. Because it is often considered an “experimental” form of treatment and can cause avoidable health risks, it is not typically in the interests of insurance companies to cover this riskier form of detox. This means that for most patients, rapid detox is a private-pay option, requiring substantial upfront out-of-pocket expenses. This can make an already challenging situation even more stressful. If you’re wondering How to pay for addiction treatment, we have resources to help you explore more affordable and covered options.
The Safer Path: Alternatives and Aftercare
Medically Supervised Detox: The Gold Standard
When it comes to safely and effectively managing opioid withdrawal, medically supervised detox is widely considered the gold standard. This approach prioritizes patient safety and comfort, offering a gradual and controlled process rather than a rushed, forced withdrawal.
In a medically supervised setting, patients receive 24/7 medical monitoring, and healthcare professionals administer comfort medications to alleviate withdrawal symptoms. This allows the body to detoxify at a more natural pace, minimizing stress and reducing the risk of severe complications. The focus is on making the process as comfortable as possible while ensuring the patient’s physical stability. This evidence-based care is typically covered by insurance and sets the foundation for lasting recovery. We encourage you to Explore our inpatient detox program to learn more about this safer alternative.
Here’s a quick comparison of rapid detox versus medically supervised detox:
| Feature | Rapid Detox | Medically Supervised Detox |
|---|---|---|
| Safety | High risk of severe complications, including death (2% fatality rate, 9% serious complications reported by CDC) | Significantly safer; 24/7 medical monitoring to manage symptoms and prevent complications. |
| Cost | $13,000 – $28,000+ out of pocket. | Varies, but often covered by insurance; more affordable options available. |
| Duration | 1-4 days (procedure itself), with some programs offering extended aftercare up to 10 days. | Typically 7-10 days, but can be longer depending on substance and individual needs. |
| Effectiveness | No more effective than traditional detox for long-term recovery; very high relapse rate if used alone. | Effective for safely clearing substances from the body; provides a stable foundation for ongoing addiction treatment. |
| Insurance | Rarely covered, considered experimental due to risks. | Often covered by major health insurance plans due to its established medical efficacy and safety. |
| Aftercare Integration | Crucial but often an additional, separate step; some centers offer post-detox retreat but not comprehensive long-term rehab. | Seamless transition to various levels of care, including inpatient rehab, outpatient programs, and therapy, which are essential for addressing the psychological aspects of addiction and preventing relapse. |
The Critical Role of Comprehensive Aftercare
It cannot be overstated: detox is only the first step on the journey to recovery. Whether you choose medically supervised detox or consider rapid detox, addressing the physical dependence is just one piece of the puzzle. Addiction is a complex disease that impacts the brain, behavior, and overall well-being.
For lasting recovery, it’s absolutely critical to engage in comprehensive aftercare that addresses the psychological aspects of addiction. This includes various Levels of Care, such as Inpatient Rehab for intensive support, Partial Hospitalization Program (PHP) for structured day treatment, and different forms of Therapy for addiction. These programs help individuals develop coping skills, understand triggers, process trauma, and build a supportive community. Many individuals also benefit from Dual Diagnosis treatment if they are struggling with co-occurring mental health conditions.
Without this crucial follow-up care, detox, rapid or otherwise, is simply a temporary pause in substance use, leaving individuals vulnerable to relapse. The real work of recovery begins after detox.
Finding the Right Help for Opioid Addiction
How to Evaluate Reputable Rapid Detox Centers
If you are still considering rapid detox centers, it’s imperative to approach this decision with extreme caution and thorough due diligence. Given the significant risks and controversies, it is vital to vet any potential provider rigorously. Here is a list of critical questions to ask and factors to consider:
- Accreditation and Licensing: Is the facility fully licensed by the state and accredited by reputable organizations like the Joint Commission on Accreditation of Healthcare Organizations (JCAHO)? This ensures adherence to high standards of care.
- Medical Staff Qualifications: Are the medical director and all physicians board-certified in anesthesiology, addiction medicine, and/or critical care? Is there a dedicated anesthesiologist on staff during the procedure?
- Facility Setting: Is the procedure performed in a full-service, JCAHO-accredited hospital within a private Intensive Care Unit (ICU) room? Be wary of centers that perform procedures in non-hospital settings or discharge patients to hotels immediately after.
- Pre-Procedure Evaluation: Is a comprehensive medical evaluation conducted at least a full day before the detox procedure to ensure physiological readiness and minimize risks?
- Continuous Monitoring: Is there 24/7 critical care monitoring by medical professionals during and immediately after the procedure?
- Transparency in Pricing: Are all costs clearly outlined upfront, including the procedure, hospital stay, and any post-detox care? Be suspicious of hidden fees.
- Comprehensive Aftercare Plan: Does the program include a structured, professionally monitored recovery period after the detox, such as a dedicated recovery retreat with medical and therapeutic support? What are the options for long-term rehabilitation and therapy?
- Substance Scope: Does the center explicitly state it only treats opioid dependence and not other substances like alcohol or benzodiazepines?
- Patient-to-Staff Ratio: What is the ratio of patients to medical staff, particularly during the critical post-procedure hours?
- Emergency Protocols: What are the emergency transfer protocols to a higher level of care if complications arise?
Historically, the most reputable programs have always emphasized these high standards, performing procedures exclusively in JCAHO-accredited hospitals with extensive pre- and post-detox care. These established protocols set a benchmark for what “safe” rapid detox should entail. When evaluating any rapid detox centers, use these benchmarks to gauge their commitment to patient safety and comprehensive care. Finding a provider that meets these criteria is essential, and our resources can help you find addiction treatment that prioritizes your well-being.
Your Next Step: Confidential Support is Available
Making an informed decision about addiction treatment is one of the most important choices you or your loved one will ever make. It involves carefully weighing the potential risks and benefits of each option. While the appeal of a “fast track” can be powerful, we urge you to prioritize safety, evidence-based care, and a clear path to long-term recovery.
At SoberSteps, we understand that navigating the complexities of addiction treatment can be overwhelming. That’s why we’re here to help. Our confidential helpline connects you with specialists who can discuss safer, evidence-based options for opioid addiction, including medically supervised detox and comprehensive rehabilitation programs. You don’t have to steer this alone. Our team is ready to listen, answer your questions, and guide you toward reliable resources that can lead to lasting freedom from addiction.
Get Help Now by reaching out to our compassionate team. For immediate, anonymous support and guidance on mental health and addiction resources, explore our Anonymous Mental Health Hotline Guide.