
No More Excuses: The Best Online NA Meetings for Support
Find accessible Online NA meetings. Get virtual support, overcome addiction barriers & call (844) 491-5566 today.

Dual Diagnosis means having both a mental health disorder and a substance use disorder at the same time. It’s also called co-occurring disorders or comorbidity.
Quick Facts About Dual Diagnosis:
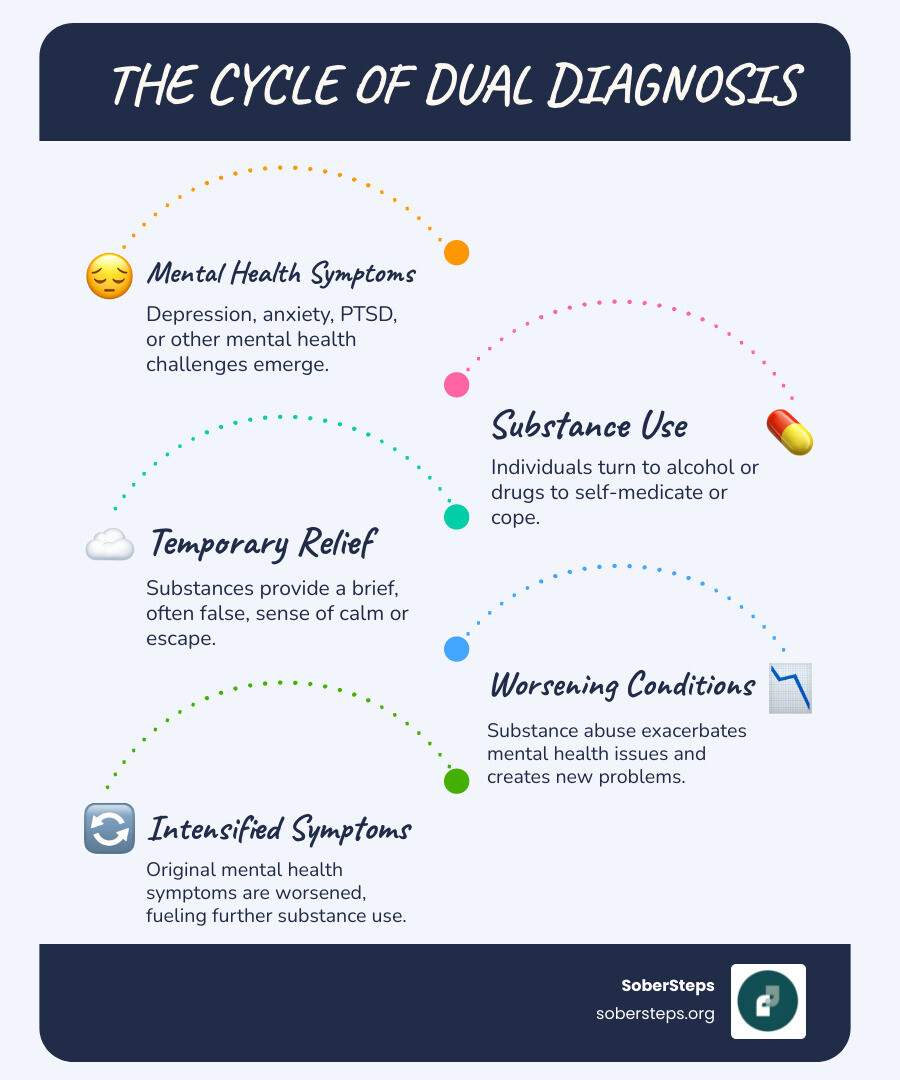
If you or someone you care about is facing this reality, you may feel trapped in a cycle where mental health symptoms lead to substance use, and substance use worsens mental health. This vicious loop is a common experience.
The statistics are clear: 37% of alcohol abusers and 53% of drug abusers also have at least one serious mental illness. Of the 21 million Americans with a substance use disorder, 8 million also live with a mental illness. You are far from alone. Many people turn to substances to cope with depression, anxiety, or trauma, only to find their symptoms worsen over time.
But here’s the most important thing to know: recovery is possible. With integrated treatment that addresses both conditions together, you can break free from this cycle and rebuild your life.
At Sober Steps, we understand the unique challenges of dual diagnosis. Our mission is to provide confidential, compassionate support and connect you with treatment options that address both conditions simultaneously, giving you the best chance for lasting recovery.
If you’re feeling overwhelmed and don’t know where to turn, you can reach our confidential helpline at (844) 491-5566 any time, day or night.
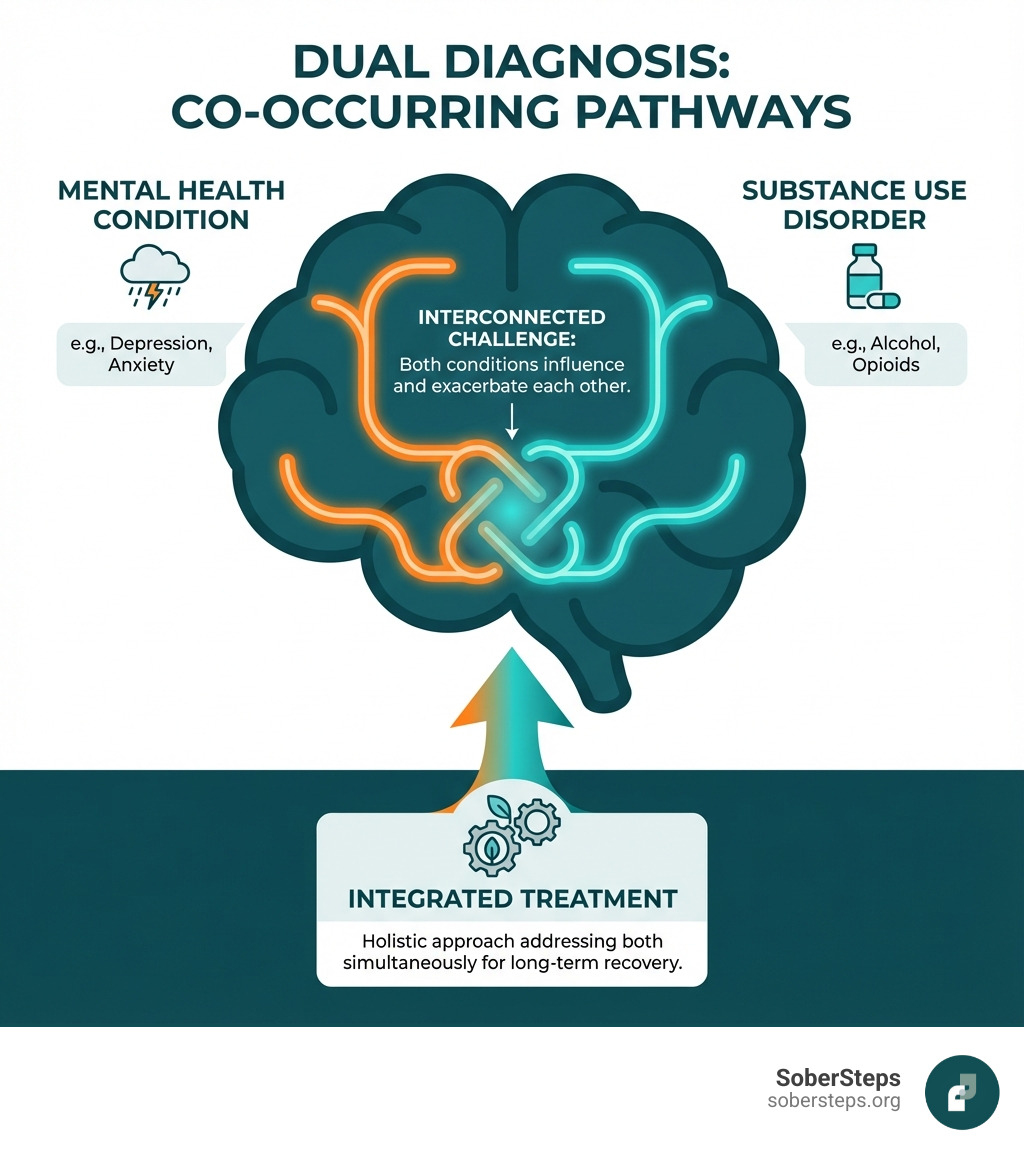
When we talk about Dual Diagnosis, we’re referring to a situation where an individual experiences both a mental health disorder and a substance use disorder (SUD) concurrently. These two conditions intertwine, influence each other, and often complicate treatment. Understanding this complex relationship is the first step toward effective recovery.
A Dual Diagnosis is the co-occurrence of a mental disorder and a substance use disorder, which can involve alcohol, illicit drugs, or prescription medications. It’s also commonly called “co-occurring disorders.”
It’s common for individuals to develop an SUD as a way to cope with the symptoms of an untreated mental illness. Conversely, prolonged substance use can alter brain chemistry, potentially triggering or worsening mental health conditions. This creates a challenging cycle that requires a specialized approach to treatment. Whether it’s an alcohol use disorder or a drug use disorder, the presence of a co-occurring mental health condition significantly impacts how both are experienced. If you’re wrestling with this, confidential help is just a phone call away at (844) 491-5566.
The numbers underscore how prevalent Dual Diagnosis is in the United States. Key statistics highlight the scope of the issue:
These figures from sources like the National Institute of Mental Health (NIMH) and SAMHSA confirm that Dual Diagnosis is a common challenge in mental health and addiction treatment. You can find more information on this topic from the National Institute of Mental Health’s page on Substance Use and Co-Occurring Mental Disorders.
Certain mental health conditions frequently appear alongside substance use disorders, often exacerbating each other.
Some of the most common co-occurring disorders include:
The relationship between mood disorders and substance use is particularly strong, creating a complex clinical picture where symptoms overlap and influence each other. Addressing both is critical for recovery.
It’s natural to wonder why mental health and substance use disorders so frequently appear together. The link is multifaceted, involving a complex interplay of biological, psychological, and environmental factors.
Researchers have identified three primary reasons why these conditions often co-occur:
Let’s dive deeper into these connections.
The self-medication hypothesis suggests that individuals use alcohol or drugs to cope with the distressing symptoms of a mental health disorder. Substances may offer a temporary escape from anxiety or depression, but this relief is short-lived. Substance use tends to worsen the underlying mental health condition. For example, someone with depression may drink to feel better, only to find their depressive symptoms intensify over time. This creates a difficult cycle that deepens both disorders and is hard to break without professional help.
Beyond self-medication, several shared risk factors can make a person more susceptible to both conditions:
Understanding these interconnected causes helps us approach Dual Diagnosis with a comprehensive and compassionate perspective.
Recognizing a Dual Diagnosis can be challenging because the symptoms of mental illness and substance use disorders often overlap. For instance, both depression and heavy alcohol use can cause fatigue and social withdrawal. Being aware of common signs is the first step toward seeking help.

If you or a loved one are experiencing several of the following, it might indicate a Dual Diagnosis:
A proper diagnosis requires a comprehensive assessment by qualified professionals to distinguish between substance-induced symptoms and an independent mental health disorder.
The diagnostic process typically involves:
The goal is to determine if symptoms are substance-induced or represent an independent mental health disorder. This distinction is vital for creating the most effective treatment plan. If you’re unsure where to start, we encourage you to call our 24/7 helpline at (844) 491-5566 for guidance.
When it comes to Dual Diagnosis, both conditions need to be treated as one. Integrated treatment is the gold standard, offering the most effective path to recovery by addressing both the mental health disorder and the substance use disorder simultaneously.
Historically, mental health and addiction were treated separately, an approach that often failed. Today, integrated treatment is the gold standard because we know both disorders must be addressed at the same time for recovery to be successful. This approach means:
The best Dual Diagnosis treatment combines care for both conditions, offering the best chance for long-term recovery.
Effective Dual Diagnosis treatment requires a custom approach that matches the intensity of care to your needs. SoberSteps can help you find the right level of care to support you, including:
Choosing the right level of care is a collaborative decision. To understand which level is best for your journey, call us at (844) 491-5566 today.
Behavioral therapies are the cornerstone of Dual Diagnosis treatment, equipping you with skills to manage both conditions. Effective approaches include:
Medication and robust support systems are also vital in managing Dual Diagnosis.
Medication-Assisted Treatment (MAT) uses FDA-approved medications with counseling to treat substance use disorders (e.g., for opioid, alcohol, and nicotine addiction). For mental health conditions, medications like antidepressants or mood stabilizers can lessen symptoms, making it easier to engage in therapy. Your treatment team will carefully manage medications to support your overall recovery goals.
Support Groups provide a safe space to connect with peers who understand your experiences. Groups like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and Dual Recovery Anonymous (DRA) foster a sense of community, reduce isolation, and remind you that you are not alone on your journey.
Starting on the path of recovery from Dual Diagnosis is a courageous journey of building a new life. While it involves ongoing effort and presents challenges, the outlook for individuals who commit to integrated treatment is overwhelmingly positive. You are not alone, and help is available 24/7 at (844) 491-5566.
Supporting someone with a Dual Diagnosis is challenging, but your role can be pivotal. Here’s how you can help:
Treating Dual Diagnosis is complex, and several challenges often arise:
With integrated treatment, the outlook for individuals with Dual Diagnosis is hopeful. While the journey requires ongoing effort, recovery is not only possible but expectable.
Here’s what the outlook includes:
At SoberSteps, we believe that every individual has the potential for a fulfilling life in recovery. Our goal is to empower you with the tools and support needed to steer this journey successfully.
A Dual Diagnosis can feel overwhelming, but integrated treatment provides a clear path to recovery. By addressing both the mental health condition and the substance use disorder simultaneously, you can reclaim control and build a healthier, more fulfilling future. The journey starts with a single, confidential step. SoberSteps is here to guide you with compassion and expertise. Don’t wait to start your recovery journey. Call our confidential helpline at (844) 491-5566 or learn more about our Levels of Care. For immediate support, call (844) 491-5566—help is available 24/7. If you or a loved one needs guidance, reach out to SoberSteps at (844) 491-5566 today.

Find accessible Online NA meetings. Get virtual support, overcome addiction barriers & call (844) 491-5566 today.
Discover safe, medically supervised withdrawal. Learn what an inpatient detox program offers for your first step to lasting recovery.
Your guide to finding a mental health clinic near you. Learn about services, insurance, veteran support, and how to get help.
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.