Cracking the Code: How to Pay for Rehab and Maximize Your Insurance
Find affordable rehab solutions. Learn how to navigate insurance, government aid, and financing for paying for rehab.
CareSource is a nonprofit health insurance organization serving over 2 million members across multiple states with government-sponsored plans that include coverage for mental health and substance use disorder treatment. Founded in 1989, CareSource is the largest Medicaid plan in Ohio and the second-largest Medicaid plan in the United States.
Quick Facts About CareSource Coverage:
If you’re struggling with substance use disorder and have CareSource insurance, you likely have coverage for addiction treatment. The extent of that coverage depends on your specific plan type, state, and the medical necessity of the treatment.
Need help navigating your benefits right now? Call our 24/7 confidential helpline at (844) 491-5566 to speak with a treatment advisor who can verify your CareSource coverage for free and help you find appropriate care.
The Affordable Care Act changed the landscape of addiction treatment by requiring most insurance plans to cover mental health and substance use disorder services. This means CareSource members have access to a range of treatment options – from medical detoxification to long-term outpatient therapy. However, understanding what your specific plan covers, finding in-network providers, and navigating pre-authorization requirements can feel overwhelming when you’re already dealing with addiction.
At Sober Steps, we specialize in helping individuals understand and maximize their insurance benefits, including CareSource plans, to access the addiction treatment they need without unnecessary barriers. Our mission is to provide confidential support and resources to guide you through every step of the recovery process.
This guide will walk you through exactly what CareSource covers for substance abuse treatment, how to verify your benefits, and the steps to enroll in appropriate care based on your specific plan and needs.
CareSource is a truly unique organization in the healthcare landscape. Founded in 1989 as a nonprofit, its original mission was to provide access to quality healthcare for vulnerable populations. From its humble beginnings, it has grown into a major player, now serving over 2 million members across seven states. This growth is a testament to its commitment to accessible care. With an annual revenue of $13.1 billion and a dedicated team of 4,500 employees, CareSource has significantly expanded its reach and impact. In fact, it has solidified its position as the largest Medicaid plan in Ohio and the second largest in the entire United States.
At its core, CareSource offers government-sponsored health plans. This means they often work in partnership with state and federal programs to deliver healthcare solutions. Their product offerings have evolved significantly since their founding to meet diverse needs. Today, they provide a range of plans, including:
The services CareSource offers are broad, encompassing everything from primary care and preventive services to specialized treatments. Critically for us, this includes extensive coverage for mental health and substance use disorder services, largely mandated by the Affordable Care Act. This commitment to comprehensive care is a cornerstone of their approach. For more detailed information about their history and mission, you can visit their official About us CareSource page.
When you’re looking at CareSource Marketplace plans, you’ll often encounter different “metal tiers”: Bronze, Silver, and Gold. Think of these tiers as different ways to share the cost of your healthcare with CareSource. They don’t necessarily indicate the quality of care, but rather how much you pay for your monthly premium versus how much you pay when you receive services.
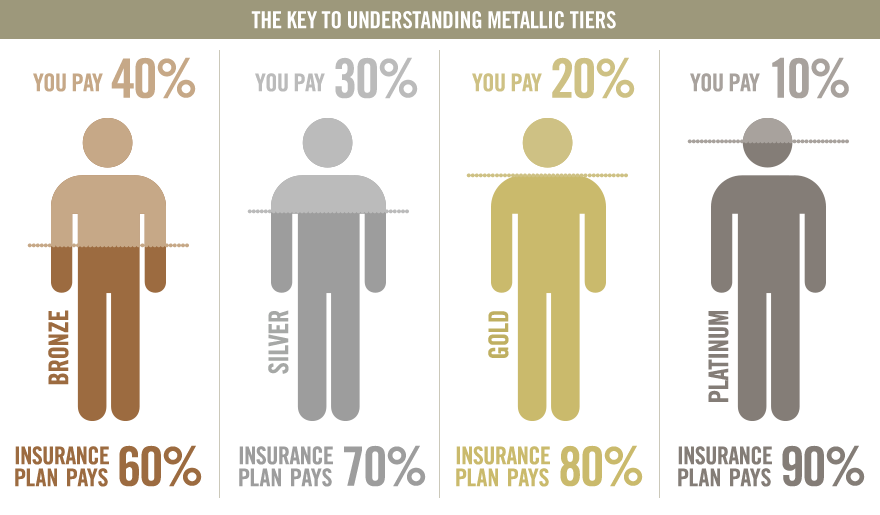
Understanding these tiers, along with terms like copays (a fixed amount you pay for a service), deductibles (the amount you must pay before your insurance starts to pay), and out-of-pocket maximums (the most you’ll have to pay in a year), is crucial. For some CareSource Medicaid plans, particularly in states like Ohio, treatment for addiction may even come with $0 cost, making it incredibly accessible.
The Affordable Care Act (ACA), signed into law in 2010, fundamentally changed how health insurance providers, including CareSource, approach coverage for mental health and substance use disorder services. Before the ACA, many insurance plans either didn’t cover these services at all or offered very limited coverage. The ACA mandated that most individual and small employer health insurance plans cover 10 “essential health benefits” (EHBs), and crucially, mental health and substance use disorder services are among them.
This means that any CareSource plan you enroll in, whether it’s a Marketplace plan, Medicaid, or a Dual plan, will include at least some coverage for addiction treatment and mental health support. This is a huge win for individuals and families struggling with these issues, as it removes a significant financial barrier to seeking help.
Furthermore, the ACA strengthened parity laws. This means that mental health and substance use disorder benefits must be offered at a level comparable to medical and surgical benefits. For example, if your plan doesn’t require pre-authorization for a physical health emergency, it generally shouldn’t require it for a mental health or substance use disorder emergency either. This ensures that treatment for addiction is treated with the same importance as any other medical condition. The ACA also prohibits insurance companies from denying coverage or charging more based on pre-existing conditions, which is particularly vital for those with ongoing substance use disorders. You can learn more about mental health and substance abuse coverage under the ACA on HealthCare.gov.
One of the most important aspects of CareSource coverage is its commitment to helping members access a full spectrum of addiction treatment services. We know that recovery isn’t a one-size-fits-all journey, and different individuals require different levels and types of care. CareSource plans, guided by the ACA’s mandates, typically cover a range of treatments, provided they are deemed medically necessary and part of an individualized treatment plan developed by a healthcare professional.
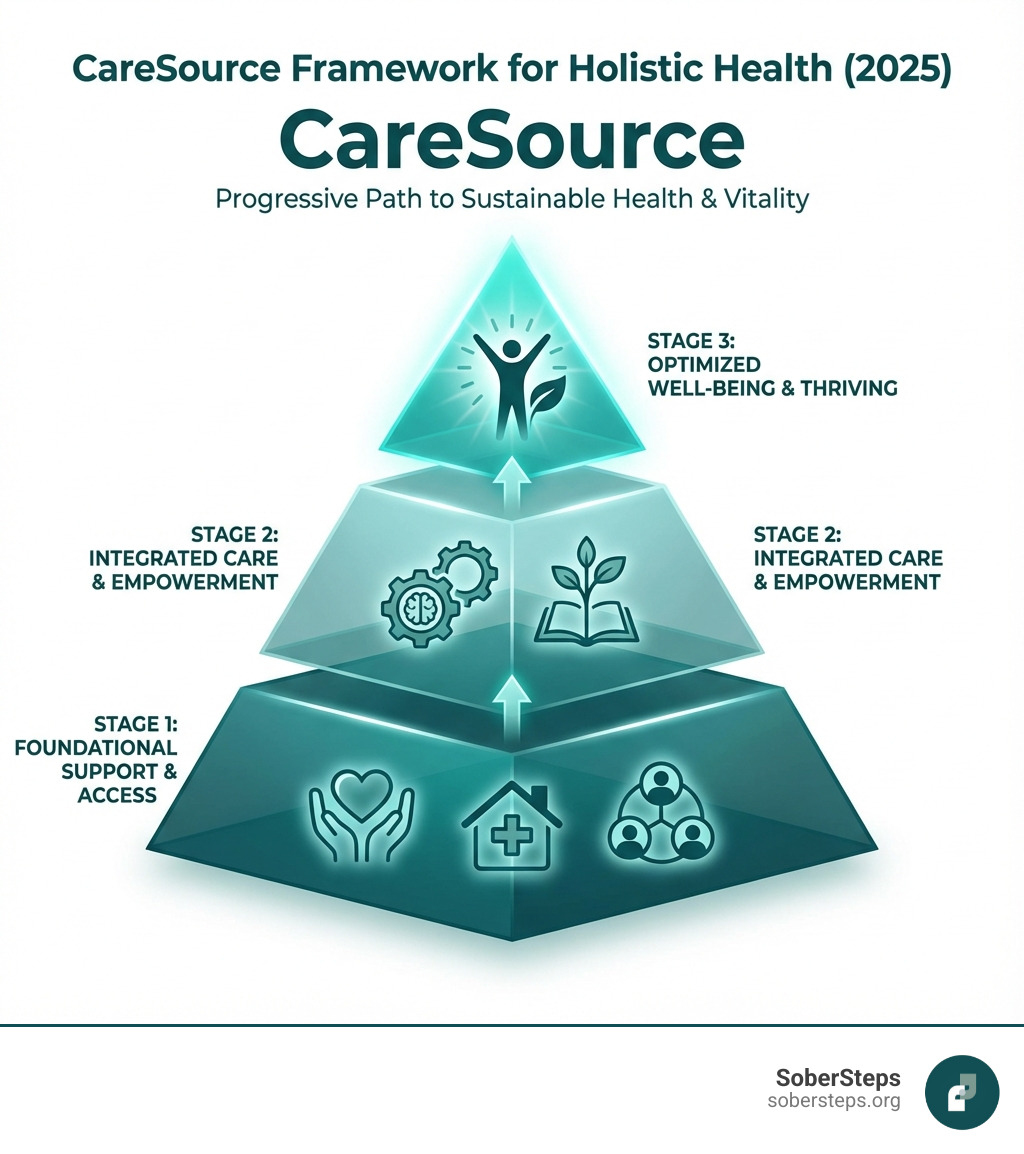
This continuum of care ensures that from the initial crisis to long-term recovery support, members have options.
Often the first critical step in overcoming substance dependence, medical detoxification is designed to safely manage the physical symptoms of withdrawal. This process can be uncomfortable, painful, and even dangerous if not medically supervised. CareSource typically covers medical detox services, recognizing their essential role in preparing an individual for further treatment.
During medical detox, you’ll receive 24/7 medical supervision and support. Healthcare professionals monitor vital signs, administer medications to alleviate withdrawal symptoms, and ensure your safety and comfort. While the average length of stay for detox is often less than 10 days, it provides a crucial foundation for recovery, allowing your body to stabilize and your mind to begin focusing on therapeutic work. For immediate help with detox, call our confidential helpline at (844) 491-5566. You can also dig into more research on detoxification and substance abuse treatment via the SAMHSA guide, Detoxification and Substance Abuse Treatment.
For many struggling with severe substance use disorder, inpatient or residential rehabilitation offers the most immersive and supportive environment for initial recovery. These programs provide a structured setting where individuals live at the facility for an extended period, typically from 30 to 90 days, or sometimes longer.
Within these programs, CareSource coverage generally extends to:
Inpatient rehab is often recommended for those with a long history of substance abuse, co-occurring mental health disorders, or those who have not found success with less intensive forms of treatment.
For individuals who require a high level of care but have stable living situations and a strong support system, or who are transitioning from inpatient treatment, CareSource covers various outpatient program levels. These programs allow you to live at home or in sober living while attending therapy and treatment sessions during the day.
The benefits of outpatient care, covered by CareSource, include:
Beyond PHP and IOP, CareSource also covers general outpatient care, which involves less frequent sessions, often once or twice a week, focusing on therapy, relapse prevention, and connecting with community resources. Telehealth options for remote treatment may also be available, depending on your plan and state.
It’s very common for individuals struggling with substance use disorder to also have a co-occurring mental health condition, such as depression, anxiety, or PTSD. This is often referred to as a “dual diagnosis.” Addressing both conditions simultaneously is crucial for successful, long-term recovery.
CareSource recognizes the importance of integrated care for co-occurring disorders. Their plans, in line with ACA mandates, typically cover specialized treatment that addresses both the mental health condition and the substance use disorder concurrently. This approach ensures that treatment for one condition doesn’t inadvertently exacerbate the other.
Integrated treatment for co-occurring disorders may include:
We understand that navigating these complex needs can be challenging, but rest assured, if you have a CareSource plan, you likely have access to the comprehensive care needed for both your mental health and substance use disorder. For more in-depth information on co-occurring disorders, refer to Information on co-occurring disorders.
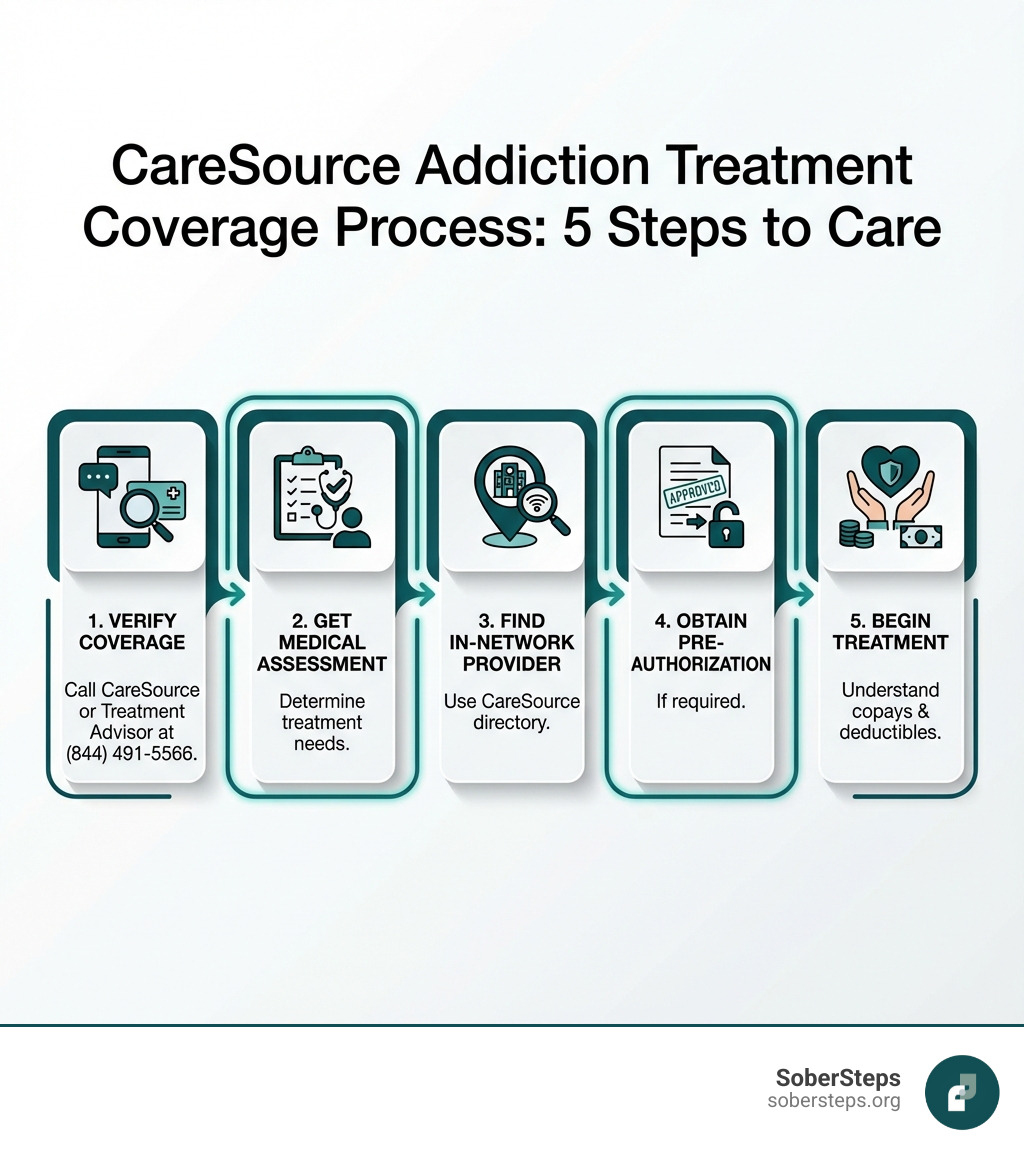
Understanding that you have CareSource coverage for addiction treatment is one thing; navigating the actual process of using it is another. It can seem daunting, but we’re here to break it down into manageable steps. Key considerations will be pre-authorization requirements and whether a facility is in-network or out-of-network.
The very first step is to get a clear picture of your specific benefits. The best way to do this is to directly contact CareSource.
The more specific information you have about your plan, the better.
Once you know what your CareSource plan covers, the next crucial step is finding a treatment facility that accepts your insurance and is “in-network.”
While CareSource plans generally prefer in-network care, out-of-network coverage might be available, but it typically comes with significantly higher out-of-pocket expenses. It’s always best to aim for in-network providers if possible.
Even with insurance coverage, you’ll likely have some financial responsibility. Understanding these costs upfront helps avoid surprises.
It’s worth reiterating that for individuals with CareSource Medicaid plans in certain states, addiction treatment may come with $0 cost, meaning you might not have any copays, deductibles, or coinsurance for covered services. This is a huge benefit and makes treatment incredibly accessible. Always verify these details with CareSource or our advisors at (844) 491-5566.
We hear a lot of common questions about CareSource coverage for addiction treatment. Here are some of the most frequent inquiries we receive, along with clear answers to help you steer your options.
Yes, generally, CareSource plans do cover medications for addiction treatment, such as Suboxone (buprenorphine/naloxone), methadone, and naltrexone. These are often referred to as Medication-Assisted Treatment (MAT), which is recognized as an evidence-based approach to treating opioid use disorder and alcohol use disorder. Since mental health and substance use disorder services, including MAT, are considered essential health benefits under the Affordable Care Act, CareSource plans are mandated to provide coverage.
However, the specifics of coverage can vary based on your individual plan, the state you’re in, and the particular medication. There might be requirements for pre-authorization, specific dosage limits, or a preference for generic versions over brand names. A medical professional will determine if MAT is appropriate for your treatment plan, and then you can work with your provider and CareSource to ensure coverage.
This is a very important question, as healthcare coverage is often state-specific. Generally, if your CareSource plan is from one state (e.g., an Ohio Medicaid plan), your coverage will primarily be for providers and services within that state. While some emergency services might be covered out-of-state, routine or planned addiction treatment usually requires you to seek care in the state where your plan is active and where CareSource operates its network for your specific plan type.
If you’ve moved or need treatment outside of your plan’s state, you might need to look into transferring your plan or obtaining new coverage in your current state of residence. This can be a complex process, but ensure your treatment is covered. For personalized guidance on navigating state-specific coverage and finding appropriate care, you can always call our specialists at (844) 491-5566. We can help you understand your options and connect you with resources.
Pre-authorization (sometimes called prior authorization or pre-certification) is a common requirement for many significant medical services, including addiction treatment programs like inpatient rehab or even certain outpatient levels of care. It means that CareSource needs to approve the treatment before you start receiving it for the services to be covered. This process ensures that the proposed treatment is medically necessary and meets CareSource’s clinical guidelines.
Typically, you won’t need to handle the pre-authorization process yourself. Your doctor or the treatment facility you plan to attend will usually manage this. They will submit a request to CareSource that includes:
It’s crucial that this pre-authorization is obtained before you begin treatment. If you start treatment without the necessary approval, CareSource may deny coverage, leaving you responsible for the full cost. Always confirm with the treatment facility that pre-authorization has been secured before admission.
Addiction is a treatable disease, and with the right support, recovery is absolutely possible. We understand that taking the first step can be incredibly challenging, especially when you’re trying to figure out the complexities of insurance coverage. However, your CareSource plan provides a clear pathway to accessing the care you need and deserve.
At SoberSteps.org, we believe in empowering individuals with the knowledge and resources to make informed decisions about their health. We provide confidential and anonymous help for mental health and substance use disorders, connecting you to the right treatment options without judgment.
Do not let worries about insurance or uncertainty about treatment options keep you from seeking help. The commitment of CareSource to covering essential health benefits, including comprehensive addiction treatment, means that financial barriers are often significantly reduced or eliminated. Your well-being is our priority, and we are here to support you every step of the way.
Call our 24/7 confidential helpline at (844) 491-5566 to speak with a treatment advisor who can verify your CareSource coverage and help you start your recovery journey today.
Learn more about your insurance options
Find affordable rehab solutions. Learn how to navigate insurance, government aid, and financing for paying for rehab.

Understanding Rapid Detox: What You Need to Know Before Deciding Rapid detox centers offer a controversial approach to opioid withdrawal that promises to eliminate the worst symptoms in just a few days.
Decode your mental health insurance. Explore coverage, laws, plan types, and steps to access care. Get empowered to use your benefits.
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.