
More Than Just Words: Understanding Dual Diagnosis and Co-Occurring Conditions
Understand dual diagnosis vs co-occurring disorders. Learn why the distinction matters for integrated treatment and find support today.
Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment is a critical resource for millions of Americans seeking help for substance use disorders. If you’re wondering whether your BCBS plan covers rehab, here’s what you need to know:
Quick Answer: Does BCBS Cover Addiction Treatment?
Navigating insurance for addiction treatment can be overwhelming. Blue Cross Blue Shield is a federation of 36 independent health insurance companies serving over 100 million people nationwide. This means your specific coverage depends on the BCBS company in your state and your selected plan.
The good news is that federal laws like the Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act (MHPAEA) mandate that BCBS plans cover mental health and substance use disorders on par with medical services. Addiction treatment is now a protected, essential service.
At Sober Steps, we help individuals understand their Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment to access life-saving care. We know the system is confusing, so we’re here to simplify it. Call us at (844) 491-5566 and let us help you take the first step toward recovery.
Blue Cross Blue Shield (BCBS) plans are required to cover addiction treatment. Federal laws like the Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act (MHPAEA) mandate that substance use disorder (SUD) treatment is an essential health benefit, meaning BCBS must provide coverage.
However, coverage specifics vary. BCBS is a federation of 36 independent health insurance companies, so your Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment depends on your local BCBS company and the specific plan you’ve chosen.
A key factor is “medical necessity.” Insurers only cover treatments deemed necessary by a healthcare professional, often requiring a diagnosis and an evidence-based treatment plan. Higher levels of care like inpatient treatment may require “pre-authorization”—permission from your insurer before starting treatment to ensure coverage and prevent unexpected costs.
The vast BCBS network covers over 100 million Americans and more than 90% of doctors and hospitals nationwide, increasing your chances of finding an in-network provider. Always verify network status, as out-of-network care costs more.
To get the most accurate information, we recommend contacting your local BCBS company directly. You can find their contact information here: Find your local BCBS company.
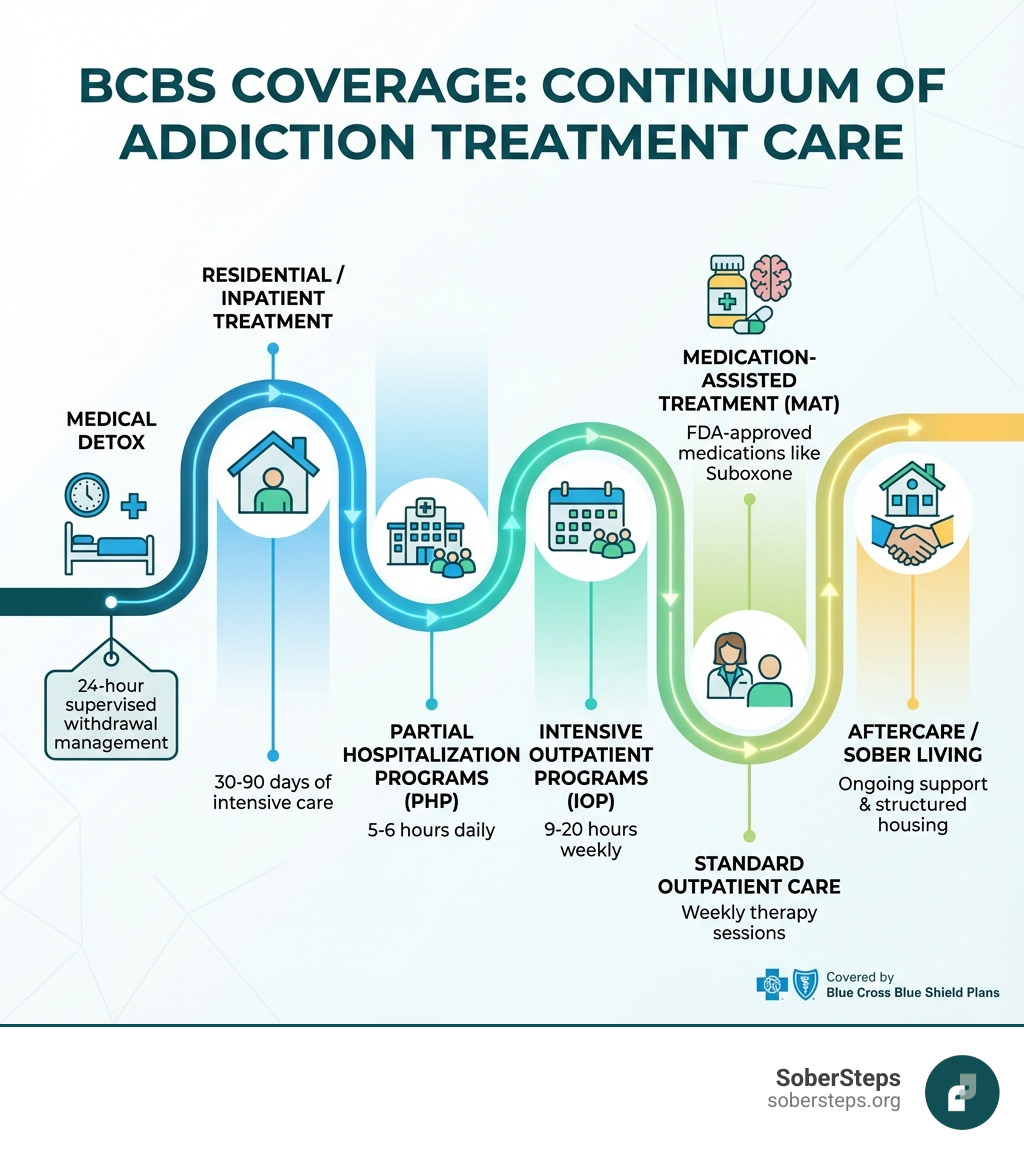
BCBS plans typically cover a comprehensive range of services to support individuals through every stage of recovery. Effective treatment often involves a multi-faceted approach.

Here’s a breakdown of the types of addiction treatment services that Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment generally includes:
BCBS plans are designed to cover treatment for a wide array of substance addictions, including:
Yes. Addiction often co-occurs with mental health conditions like depression, anxiety, or PTSD, known as a “dual diagnosis.” These conditions can significantly impact recovery.
The good news is that Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment typically covers co-occurring disorders. Federal parity laws mandate that mental health care, including SUD treatment, must be covered at the same level as physical health care.
BCBS plans treat behavioral health conditions and substance use disorders, including integrated care for co-occurring conditions. This means if you are seeking treatment for both an addiction and a mental health issue, your BCBS plan should cover services that address both simultaneously. Such integrated treatment is considered best practice and often includes:
Coverage for co-occurring disorders is still subject to medical necessity criteria. When seeking help, find a treatment center that specializes in dual diagnosis to ensure you receive comprehensive care.
Understanding the financial side of your Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment is key. Let’s break down deductibles, co-pays, and coinsurance—the main parts of your out-of-pocket costs.

These costs vary significantly by plan. For a deeper dive, BCBS provides a helpful resource: How deductibles and copays work.
BCBS, like other insurers on the Health Insurance Marketplace, categorizes plans into “metal tiers”: Bronze, Silver, Gold, and Platinum. These tiers indicate how you and your plan share costs. It’s a balance between your monthly premium and what you pay when you need care.
Here’s a general overview of how these tiers typically affect your Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment:
| Plan Tier | Typical Coverage % (after deductible) | Monthly Premium | Deductible Level | Out-of-Pocket Costs |
|---|---|---|---|---|
| Bronze | Approximately 60% | Lowest | Highest | Highest |
| Silver | Approximately 70% | Moderate | Moderate | Moderate |
| Gold | Approximately 80% | High | Low | Low |
| Platinum | Approximately 90% | Highest | Lowest | Lowest |
Let’s break it down:
Understanding these tiers is crucial. A plan with a lower premium might seem attractive, but if you need extensive addiction treatment, a higher-tier plan could ultimately save you thousands in out-of-pocket expenses. For more detailed information on these tiers, you can visit Understanding Insurance Tiers.
You’ve taken the courageous step to seek help. Now, let’s figure out how your Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment can support you. Verifying benefits is the next step, and we can guide you.
Understanding the difference between in-network and out-of-network providers is critical. BCBS negotiates rates with in-network providers, so using them results in lower out-of-pocket costs. Choosing an out-of-network provider means higher costs, and some services may not be covered, depending on your plan (HMO vs. PPO).
Using an in-network provider is the most cost-effective option. Some BCBS plans feature “Blue Distinction Centers” for substance use treatment, recognized for high-quality care. Always verify any center’s in-network status with your specific plan.
At SoberSteps, we understand this can be a lot to steer. Our admissions support team is here to assist you every step of the way.
Verifying your BCBS coverage is crucial to understand covered services, out-of-pocket costs, and pre-authorization needs. Here’s how:
If your Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment doesn’t cover the full cost, treatment is still within reach. There are several alternative options to explore:
The key is to communicate openly with the treatment facility’s admissions team. They can help you explore all available options and create a plan that works for you. There are always pathways to recovery, and we are here to help you find them. Call us at (844) 491-5566 to explore your options.
Navigating insurance can bring up a lot of questions. Here, we address some of the most common inquiries about Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment.
The best way is to call the member services number on your BCBS card or use the provider directory on your local BCBS website. You can also ask the SoberSteps admissions team to verify this for you at (844) 491-5566.
Yes, most BCBS plans cover Medication-Assisted Treatment (MAT), including FDA-approved medications like Suboxone, methadone, and Vivitrol, when medically necessary. As an evidence-based approach, MAT is widely supported by BCBS. Your specific plan’s prescription benefits will determine the extent of coverage.
Pre-authorization (or prior approval) is your insurer’s requirement for approval before you receive a service to ensure it’s medically necessary and covered. Higher levels of care, like inpatient rehab, often require it for your Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment to apply. Your provider usually handles this, but it’s wise to confirm it’s secured. If you’re unsure, call us at (844) 491-5566 for guidance.
BCBS covers medically necessary treatments. While luxury centers offer excellent care, the “luxury” aspects (e.g., upscale amenities, private chefs) are not typically covered. Your plan will likely cover the clinical components (therapy, medical care) if the facility is in-network and the care is medically necessary. You may be responsible for the cost of premium amenities. Verify coverage with your BCBS plan and the facility to understand your out-of-pocket expenses.
BCBS offers various plans that integrate with government programs:
In both cases, coverage depends on your specific BCBS plan and state program rules.
BCBS offers several resources beyond direct coverage:
These resources are designed to empower you and help you connect with the care you need.
Understanding your Blue Cross Blue Shield Health Insurance: Coverage for Addiction Treatment is a powerful first step, but taking action is the most important one. At SoberSteps.org, we are dedicated to providing confidential and anonymous help for mental health and substance use disorders. We understand the courage it takes to seek treatment, and we’re here to simplify the process.
We know that navigating insurance, finding the right treatment center, and understanding financial options can be overwhelming. Our mission is to be your trusted resource, offering clear, compassionate guidance without judgment.
If you or a loved one is struggling with addiction, don’t let the complexities of insurance deter you. We can help you verify your benefits, explore treatment options, and connect you with the support you need. For immediate, confidential assistance in verifying your benefits and finding the right treatment, call SoberSteps at (844) 491-5566.
Your journey to recovery starts here. Let us help you take that crucial next step. Call SoberSteps at (844) 491-5566 to get started.
Find out more about using your insurance for treatment

Understand dual diagnosis vs co-occurring disorders. Learn why the distinction matters for integrated treatment and find support today.
Explore the real connection between ADHD and substance use. Debunk myths, understand risks, and discover effective treatment for a hopeful future.
Find comprehensive cocaine addiction treatment. Understand symptoms, withdrawal, and effective therapies for lasting recovery. Get help.
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.