Understanding the Critical First Step to Recovery
Alcohol Withdrawal is a set of physical and mental symptoms that occur when someone who has been drinking heavily for weeks, months, or years suddenly stops or significantly reduces their alcohol intake. If you’re experiencing symptoms or considering quitting, here’s what you need to know right now:
Key Facts About Alcohol Withdrawal:
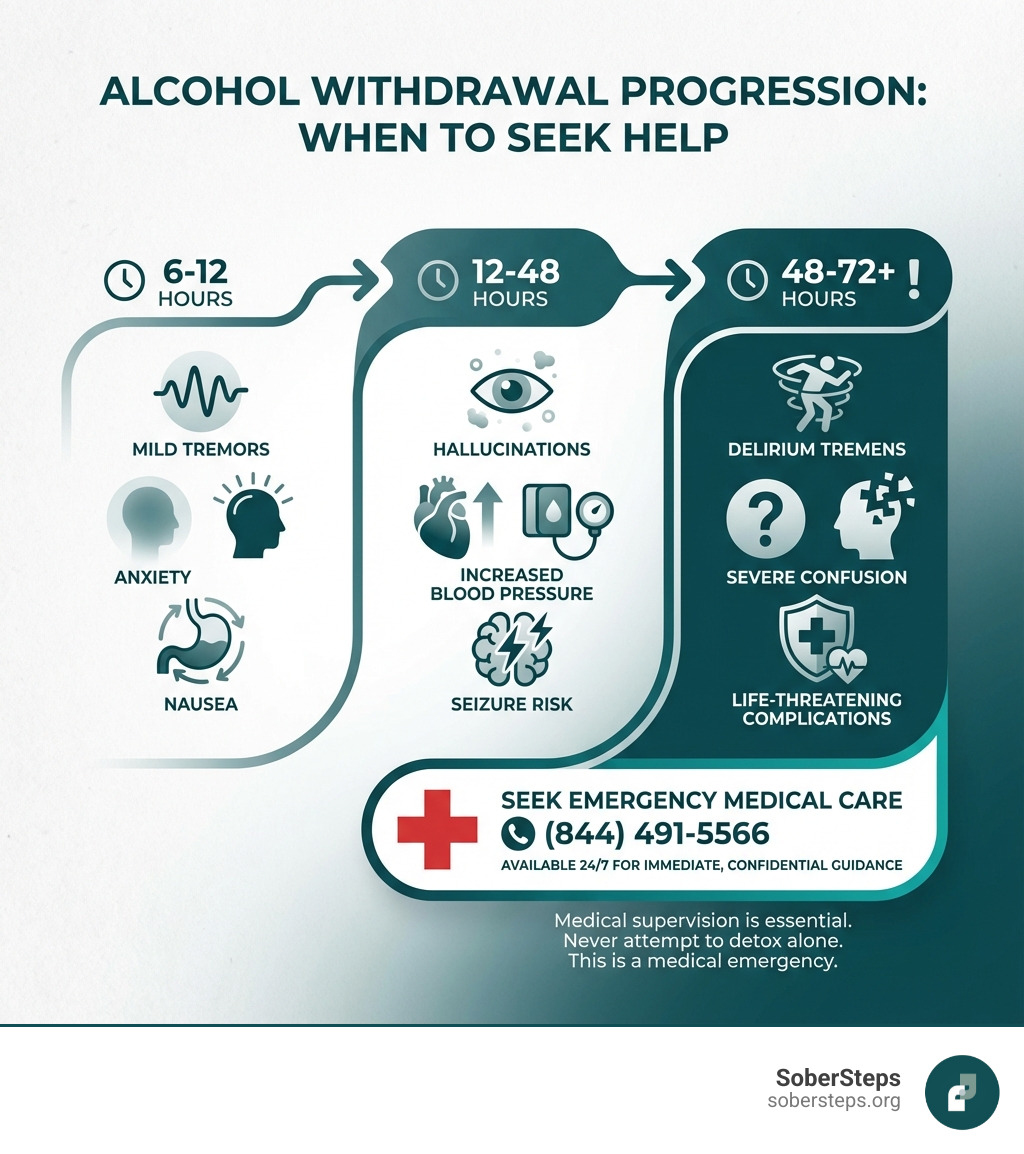
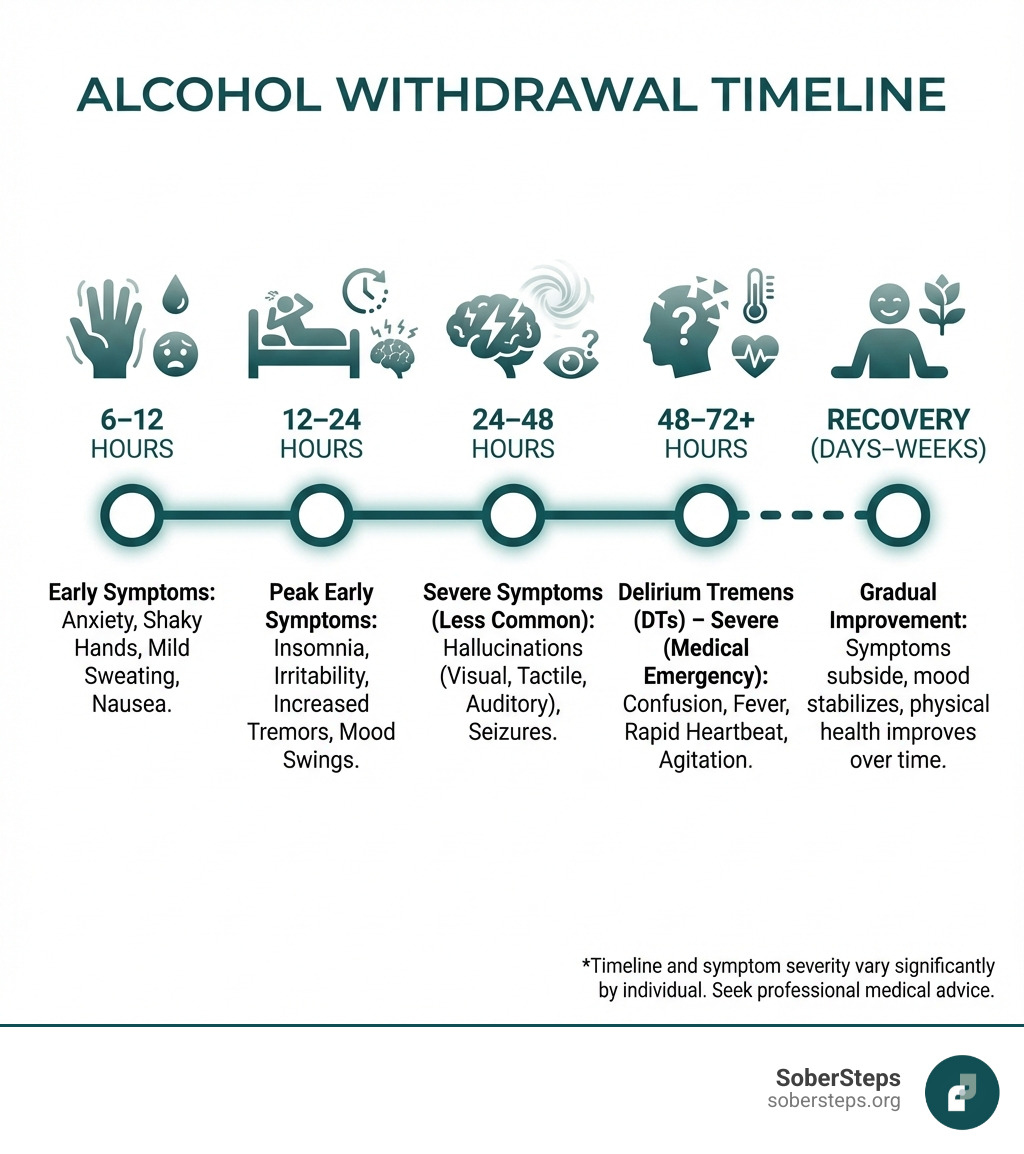
- Symptoms typically start 6-12 hours after your last drink
- Peak severity occurs at 24-72 hours
- Common symptoms include tremors, anxiety, sweating, nausea, rapid heart rate, and confusion
- Severe complications can include seizures and delirium tremens (DTs), which can be fatal
- Medical supervision is essential – approximately 500,000 Americans require medical treatment for severe withdrawal episodes each year
- Never attempt to detox alone – up to 15% of those with untreated severe symptoms may die
This is a medical emergency that requires professional help. Call (844) 491-5566 now for immediate, confidential guidance.
Alcohol acts as a depressant on your central nervous system. When you drink heavily over time, your brain adapts to the constant presence of alcohol. When you suddenly stop, your brain becomes overactive—like a car with a stuck accelerator. This hyperactivity causes withdrawal symptoms that range from uncomfortable to life-threatening.
The statistics paint a sobering picture. More than 1.5 million people in the United States go through alcohol withdrawal in a medical or rehab setting each year. About half of people with alcohol dependence will experience withdrawal symptoms when they stop drinking, and 3-10% will experience severe, potentially deadly withdrawal. The good news? With proper medical treatment, the mortality rate for severe withdrawal has dropped from 20% to about 1%.
If you’re experiencing any withdrawal symptoms, don’t wait. Call (844) 491-5566 for a confidential assessment available 24/7.
The severity of withdrawal varies greatly from person to person. Risk factors include how much and how long you’ve been drinking, previous withdrawal episodes, your age (especially over 65), co-existing health conditions, and family history. Older adults face particular risk—they can experience severe withdrawal even with moderate alcohol consumption due to slower metabolism and other health factors.
One particularly concerning phenomenon is called “kindling.” Each time you go through withdrawal, your brain becomes more sensitive to future withdrawal episodes. This means subsequent withdrawals can become progressively more severe, with an increased risk of seizures. This is why getting professional help the first time is so important.
At SoberSteps, we understand the fear and uncertainty you’re facing right now because we’ve dedicated ourselves to helping thousands of individuals steer the complexities of Alcohol Withdrawal and recovery from substance use disorders. Our confidential platform connects you with treatment options and support, ensuring you don’t have to face this challenge alone. Call (844) 491-5566 for immediate, confidential help.
Understanding Alcohol Withdrawal Syndrome
Alcohol Withdrawal Syndrome (AWS) is a complex and potentially dangerous condition that arises when an individual who has developed physical dependence on alcohol suddenly reduces or stops their alcohol intake. To truly grasp the gravity of AWS, we need to dig into its underlying mechanisms and the factors that increase its severity.
What Causes Alcohol Withdrawal?
At its core, Alcohol Withdrawal is a neurobiological phenomenon. Alcohol is a central nervous system (CNS) depressant. This means it slows down brain activity. When someone drinks heavily and consistently, their brain adapts to this constant depressant effect. It essentially “ramps up” its own activity to compensate and maintain a state of equilibrium.
This adaptation involves key neurotransmitter systems:
- GABA System: Alcohol improves the effects of gamma-aminobutyric acid (GABA), the brain’s primary inhibitory neurotransmitter. Chronic alcohol use leads to the brain becoming less sensitive to GABA’s calming effects. When alcohol is removed, this reduced sensitivity means there’s less “braking” action in the brain.
- NMDA System: Alcohol also inhibits the activity of N-methyl-D-aspartate (NMDA) receptors, which are involved in excitatory signaling. Prolonged alcohol exposure leads to an upregulation or increased sensitivity of these receptors. When alcohol is suddenly absent, these overactive NMDA receptors contribute to an excitatory surge, like pressing the accelerator without the brakes.
The result of this delicate balance being disrupted is a state of CNS hyperexcitability. The brain, accustomed to the depressant effect of alcohol, becomes overstimulated and struggles to regulate itself without it. This overactivity manifests as the wide range of Alcohol Withdrawal symptoms.
The severity of withdrawal can be influenced by several factors, including the amount and duration of drinking. The U.S. National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines heavy drinking for males as consuming five or more drinks on any day or 15 or more per week, and for females as four or more drinks on any day or 8 or more per week. Individuals who consistently exceed these thresholds for extended periods are at higher risk. Genetic predisposition may also play a role in why some individuals experience more severe withdrawal symptoms than others.
The Kindling Effect and Withdrawal in Older Adults
The “kindling effect” is a critical concept in understanding Alcohol Withdrawal. It describes a phenomenon where repeated episodes of alcohol withdrawal lead to increasingly severe symptoms with each subsequent withdrawal. Imagine striking a match multiple times; each strike makes it easier for the flame to ignite. Similarly, each time the brain experiences the hyperexcitability of withdrawal, it becomes more sensitized, and future withdrawal episodes can be more intense, with a higher risk of complications like seizures. This makes early and comprehensive treatment crucial.
Older adults face unique challenges during Alcohol Withdrawal. They can develop significant withdrawal symptoms even with lower levels of alcohol consumption compared to younger individuals. This is due to several factors:
- Slower Metabolism: As we age, our bodies metabolize alcohol less efficiently, meaning alcohol stays in the system longer and its effects are more pronounced.
- Co-existing Health Conditions: Older adults are more likely to have other medical conditions and take medications that can complicate withdrawal or interact negatively with treatment.
- Reduced Body Water: Older adults often have less total body water, leading to higher blood alcohol concentrations for the same amount of alcohol consumed.
These factors mean that what might be considered moderate drinking for a younger person could lead to severe Alcohol Withdrawal in an older adult. If you or a loved one are struggling and fall into this vulnerable group, please call (844) 491-5566 for guidance and support.
The Typical Timeline and Symptoms of Alcohol Withdrawal
Understanding the typical timeline of Alcohol Withdrawal symptoms can help you recognize the signs and seek timely help. While individual experiences vary based on factors like drinking history, overall health, and genetic predisposition, a general progression of symptoms is often observed. It’s important to differentiate these symptoms from general anxiety, as the physiological markers of withdrawal (like tremors and rapid heart rate) are often more pronounced and directly linked to the cessation of alcohol. For a confidential assessment, call our 24/7 helpline at (844) 491-5566.
Stage 1: Mild Symptoms (6-12 Hours)
The initial phase of Alcohol Withdrawal typically begins within 6 to 12 hours after the last drink. These symptoms are generally uncomfortable but not usually life-threatening. They include:
- Anxiety and irritability: A feeling of unease, nervousness, or agitation.
- Insomnia: Difficulty falling or staying asleep, often accompanied by vivid dreams or nightmares.
- Mild tremors (the “shakes”): Involuntary shaking, particularly in the hands. This is one of the most reliable physical signs of withdrawal.
- Headache: Often a throbbing sensation.
- Nausea and vomiting: Stomach upset and potential expulsion of stomach contents.
- Sweating: Excessive perspiration, even in cool environments.
- Heart palpitations: A sensation of a racing or pounding heart.
At this stage, a person might still try to manage symptoms on their own, but medical supervision is highly recommended to prevent progression to more severe stages.
Stage 2: Moderate Symptoms & Hallucinations (12-48 Hours)
As Alcohol Withdrawal progresses, symptoms become more intense and potentially dangerous, typically appearing between 12 and 48 hours after the last drink. This stage is characterized by:
- Increased blood pressure and heart rate: The body’s autonomic nervous system becomes overactive, leading to cardiovascular stress.
- Confusion: Difficulty thinking clearly or disorientation.
- Worsening tremors: Shaking becomes more pronounced and widespread.
- Alcoholic hallucinosis: This involves experiencing hallucinations—seeing, hearing, or feeling things that aren’t there—while the person is still generally aware of their surroundings. These can be:
- Visual: Seeing objects, people, or patterns that don’t exist, sometimes described as “bugs crawling on the skin.”
- Auditory: Hearing voices, music, or other sounds.
- Tactile: Feeling sensations on the skin, like crawling insects.
- Seizure risk begins: Alcohol withdrawal seizures, often grand mal seizures, can occur during this window, typically between 24-48 hours after the last drink. These seizures are a serious complication and require immediate medical attention. Approximately 3-5% of people with alcoholism experience grand mal seizures during withdrawal.
Stage 3: Severe Symptoms (48-72+ Hours)
The most severe and life-threatening symptoms of Alcohol Withdrawal typically emerge 48 to 72 hours after the last drink, though they can sometimes be delayed for more than a week. This stage is dominated by:
- Delirium Tremens (DTs): This is the most dangerous form of alcohol withdrawal, a medical emergency characterized by profound confusion, agitation, disorientation, and autonomic hyperactivity. We’ll dig deeper into DTs next.
- Severe disorientation and confusion: The person may lose touch with reality, not knowing where they are or who they are.
- Agitation and extreme excitement: Intense restlessness and hyperactivity.
- Fever: High body temperature.
- Grand mal seizures: Repeated or prolonged seizures can lead to further complications, including brain damage or death.
- Risk of fatality: Without proper medical intervention, this stage carries a significant risk of death due to complications like respiratory arrest, cardiac arrhythmias, and uncontrolled hyperthermia.
Severe Complications: From Seizures to Delirium Tremens

The progression of Alcohol Withdrawal from mild discomfort to severe, life-threatening complications underscores the critical need for medical supervision. Untreated withdrawal is not just unpleasant; it can be fatal. Historically, the mortality rate for Delirium Tremens was as high as 20%, but with advances in critical care and prompt treatment, this rate has significantly decreased to about 1%. However, this stark improvement relies entirely on access to and utilization of medical care. The necessity of inpatient medical care for severe cases cannot be overstated. If you see these signs, call 911 immediately and then contact us at (844) 491-5566 for next steps and ongoing support.
Delirium Tremens (DTs)
Delirium Tremens, often referred to as DTs, is the most severe manifestation of Alcohol Withdrawal. It occurs in approximately 5% of patients who experience alcohol withdrawal, typically starting 48 to 96 hours after the last drink, but can be delayed up to 7-10 days. DTs is characterized by a dangerous combination of symptoms:
- Profound confusion and disorientation: Patients may be unable to recognize people or places, and may experience fluctuating levels of consciousness.
- Agitation and extreme excitement: Intense restlessness, irritability, and sometimes aggressive behavior.
- Hallucinations: Unlike alcoholic hallucinosis where the individual is aware of the unreality of their perceptions, in DTs, hallucinations are vivid, frightening, and feel very real.
- Autonomic hyperactivity: This includes dangerously high blood pressure, rapid heart rate (tachycardia), profuse sweating, and fever.
DTs is a medical emergency that requires immediate, often ICU-level, care. Without treatment, complications such as respiratory failure, cardiac arrest, and severe electrolyte imbalances can lead to death. For more information on Delirium Tremens, you can refer to authoritative medical resources like MedlinePlus: More information on Delirium Tremens.
Protracted Alcohol Withdrawal Syndrome (PAWS)
While acute Alcohol Withdrawal symptoms typically subside within a week, some individuals experience a longer-lasting set of symptoms known as Protracted Alcohol Withdrawal Syndrome (PAWS), or post-acute withdrawal. PAWS can persist for weeks, months, or even years after the acute phase. These symptoms often ebb and flow, triggered by stress, and can be frustrating and challenging for individuals trying to maintain sobriety.
Common symptoms of PAWS include:
- Mood swings: Unpredictable shifts between highs and lows.
- Sleep disturbances: Chronic insomnia, fragmented sleep, or vivid dreams.
- Fatigue: Persistent tiredness and lack of energy.
- Anhedonia: The inability to experience pleasure from activities that were once enjoyable.
- Difficulty concentrating and memory issues: “Brain fog” and problems with cognitive function.
- Increased sensitivity to stress: Heightened reactions to everyday stressors.
- Intense cravings: Persistent urges to drink, even after the physical withdrawal has passed.
PAWS is a major factor in relapse, as individuals may turn back to alcohol to alleviate these lingering, uncomfortable symptoms. Recognizing and preparing for PAWS is crucial for long-term recovery. It requires ongoing support, therapy, and the development of healthy coping mechanisms.
Medical Management and Treatment Options
Managing Alcohol Withdrawal effectively involves a comprehensive approach focused on patient safety, symptom alleviation, and preventing complications. The chosen treatment setting—inpatient or outpatient—depends heavily on the severity of withdrawal symptoms, the individual’s medical history, and the presence of risk factors for severe withdrawal.
Diagnosis of withdrawal severity is typically done using standardized tools like the Clinical Institute Withdrawal Assessment for Alcohol, Revised (CIWA-Ar) scale. This scale assesses 10 common withdrawal symptoms (nausea/vomiting, tremor, paroxysmal sweats, anxiety, agitation, tactile disturbances, auditory disturbances, visual disturbances, headache, and orientation) and assigns a score. A CIWA-Ar score of 8 or less indicates mild withdrawal, 8-15 is moderate, and above 15 signifies severe withdrawal. This objective assessment helps healthcare providers tailor treatment plans.
For mild withdrawal without significant risk factors, outpatient treatment with close monitoring and a supportive home environment might be considered. However, for moderate to severe withdrawal, or for individuals with a history of seizures, DTs, significant co-occurring medical conditions, or lack of social support, inpatient medical detox is essential.
Supportive care is a cornerstone of Alcohol Withdrawal management, regardless of severity. This includes:
- Hydration and nutrition: Alcohol use often leads to dehydration and nutritional deficiencies. Intravenous fluids and a balanced diet are crucial.
- Creating a quiet, low-stimulation environment: A calm setting with minimal noise and soft lighting can help reduce anxiety and agitation, especially during hallucinations or delirium.
- Close monitoring: Regular checks of vital signs (heart rate, blood pressure, temperature) and symptom assessment are paramount to track progress and detect complications early.
The Role of Benzodiazepines and Other Medications
Medications play a vital role in making Alcohol Withdrawal safe and manageable.
Benzodiazepines are considered the gold standard for treating AWS. They work by enhancing the effects of GABA, counteracting the brain’s hyperexcitability. Common benzodiazepines used include:
- Chlordiazepoxide and Diazepam: These are long-acting benzodiazepines often used in fixed-dose regimens or symptom-triggered protocols.
- Lorazepam: A shorter-acting benzodiazepine, often preferred for individuals with liver issues due to its different metabolic pathway.
Treatment regimens can be:
- Symptom-triggered: Medication is given only when CIWA-Ar scores reach a certain threshold. This often leads to less medication being used and shorter treatment durations.
- Fixed-dose: Medication is given at regular intervals, often with additional doses available if symptoms worsen. This may be preferred for individuals at high risk for severe complications or those who cannot reliably report symptoms.
Anticonvulsants like Gabapentin and Carbamazepine can also be used as adjuncts to benzodiazepines or as alternatives in specific situations. They can help reduce seizure risk and manage some withdrawal symptoms.
Essential Vitamins and Supplements for Alcohol Withdrawal
Chronic alcohol use depletes essential nutrients, which can worsen withdrawal symptoms and lead to serious medical complications. Replenishing these is a critical part of treatment:
- Thiamine (Vitamin B1): This is perhaps the most critical supplement. Thiamine deficiency is common in individuals with alcohol use disorder and can lead to Wernicke-Korsakoff Syndrome, a severe neurological disorder characterized by confusion, ataxia (loss of coordination), and ophthalmoplegia (eye movement abnormalities). Thiamine is administered intravenously or intramuscularly, before any glucose-containing fluids or food, to prevent worsening of this condition.
- Folic acid and multivitamins: These help address general nutritional deficiencies.
- Magnesium: Magnesium levels are often low in individuals with alcohol dependence. Supplementation can help reduce tremors, anxiety, and improve sleep.
Long-Term Recovery and Relapse Prevention
Successfully navigating Alcohol Withdrawal is a monumental first step, but it is just that—a first step. The prognosis for individuals experiencing Alcohol Withdrawal improves significantly with proper medical treatment. However, addressing the underlying Alcohol Use Disorder (AUD) is key to sustained recovery. The journey doesn’t end after detox; it’s where the deeper work begins to build a foundation for lasting sobriety. Call (844) 491-5566 to learn about long-term treatment programs and how we can support you beyond acute withdrawal.
Medications to Prevent Relapse
After detoxification, several medications are FDA-approved to help individuals maintain sobriety and prevent relapse by reducing cravings or creating an aversion to alcohol:
- Naltrexone: This medication blocks the opioid receptors in the brain that are involved in the rewarding effects of alcohol, reducing cravings and the pleasure derived from drinking. It can be taken orally or as an injectable, extended-release formulation.
- Acamprosate: This medication helps restore the balance of neurotransmitters in the brain that are disrupted by chronic alcohol use, reducing post-acute withdrawal symptoms like anxiety and sleep disturbances that can trigger relapse.
- Disulfiram: This medication works by causing an unpleasant reaction (nausea, vomiting, headache, flushing) when alcohol is consumed, thus deterring drinking. It acts as a strong deterrent and requires a commitment from the individual.
These medications are most effective when used as part of a comprehensive treatment plan that includes therapy and support.
The Importance of Therapy and Support
Beyond medication, robust psychosocial support is crucial for long-term recovery:
- Cognitive Behavioral Therapy (CBT): This therapy helps individuals identify and change negative thought patterns and behaviors that contribute to alcohol use. It equips them with coping mechanisms to handle triggers and stress without resorting to drinking.
- Support groups (e.g., Alcoholics Anonymous – AA): Groups like AA provide a community of peers who share similar experiences, offering empathy, accountability, and a structured path to recovery. Studies show that attendance at AA can significantly improve chances of sustained abstinence. For instance, 44% of those who remain free of alcohol for one year with AA attendance probably will remain abstinent for another year, a figure that increases to 91% for those abstinent for five years or more.
- Family therapy: Alcohol use disorder affects the entire family system. Family therapy helps address communication breakdowns, heal relationships, and build a supportive home environment conducive to recovery.
- Developing healthy coping mechanisms: Learning new ways to manage stress, emotions, and cravings is fundamental to preventing relapse. This can include mindfulness, exercise, hobbies, and developing a strong support network.
Frequently Asked Questions about Alcohol Withdrawal
Can you die from alcohol withdrawal?
Yes, severe, untreated Alcohol Withdrawal, particularly Delirium Tremens, can be fatal due to complications like seizures, respiratory arrest, and cardiac arrhythmias. This is why medical supervision is essential. While the mortality rate for DTs has dropped significantly with modern medical care (from 20% to about 1%), attempting to detox alone without professional help remains extremely dangerous.
How long does acute alcohol withdrawal last?
Acute withdrawal symptoms typically begin 6-12 hours after the last drink, peak within 24-72 hours, and generally subside within 5-7 days. However, some symptoms can linger in what is known as Protracted Alcohol Withdrawal Syndrome (PAWS), which can last for weeks, months, or even years.
Can I detox from alcohol at home safely?
Detoxing at home is only considered for very mild cases with no history of severe withdrawal (like seizures or DTs) and with a supportive person present 24/7 who can monitor for worsening symptoms and seek emergency care. For most people, especially those with a history of heavy drinking, a medical detoxification facility or hospital is the only safe option to manage potentially life-threatening complications. Quitting “cold turkey” without medical assistance can be extremely dangerous.
Your Confidential Path to Recovery
Alcohol Withdrawal is a serious medical condition that marks a critical turning point. It is the first, challenging step toward reclaiming your life from alcohol dependence. Professional medical and psychological support is not just helpful—it is vital for your safety and long-term success. SoberSteps provides a confidential and anonymous platform to connect you with the help you need, without judgment. Take the first step today by calling (844) 491-5566 or exploring our resources online. Find the right support for you.