The Critical Link Between ADHD and Substance Use You Need to Understand
ADHD and substance use are closely linked, a relationship vital for anyone affected by ADHD. Here are the key facts:
Key Facts:
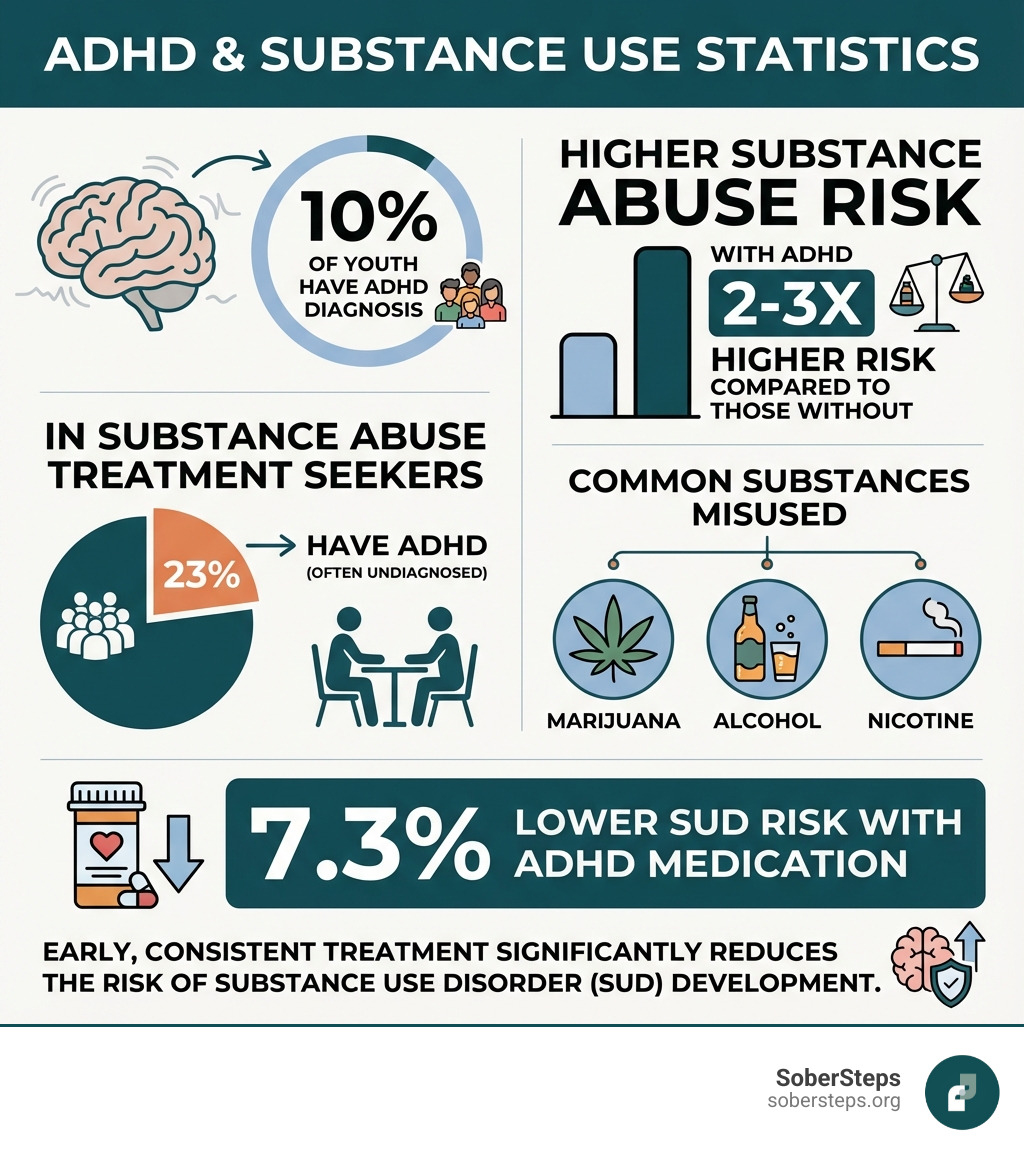
- Teenagers with ADHD are 2-3 times more likely to abuse substances.
- Common substances include marijuana, alcohol, and nicotine.
- Co-occurring mental health disorders like anxiety or depression increase the risk further.
- Early, consistent ADHD treatment reduces substance use risk by 7.3%, contrary to common fears.
- The risk is highest when ADHD is undiagnosed and untreated.
Childhood ADHD is a major risk factor for developing a substance use disorder (SUD)—the compulsive use of substances despite negative consequences. Studies show that nearly one in four patients in SUD treatment also have ADHD, which often goes undiagnosed.
But there is hope. This does not have to be your story. With proper understanding and early intervention, the risk can be significantly reduced. Treatment works, and countless individuals with ADHD live fulfilling, substance-free lives.
At Sober Steps, we support families navigating the intersection of ADHD and substance use. We provide evidence-based resources and confidential guidance for those seeking treatment for co-occurring disorders. Knowledge is the first step toward prevention and recovery.
Explore confidential treatment options for co-occurring ADHD and substance use disorders or speak with a compassionate advisor now.
Understanding the Connection: Why ADHD Increases Substance Use Risk
The link between ADHD and substance use is a complex mix of neurological, psychological, and environmental factors. People with Attention-Deficit/Hyperactivity Disorder (ADHD) have a much higher risk of developing substance use disorders (SUDs). This heightened risk isn’t about a lack of willpower; it’s rooted in the nature of ADHD itself, making it a critical issue to address for prevention and management.

The Role of Core ADHD Symptoms
The hallmark symptoms of ADHD—inattention, hyperactivity, and impulsivity—create challenges that can push individuals toward substance use.
Impulsivity is a primary driver. It manifests as:
- Poor Decision-Making: Acting on impulse can lead to substance experimentation without considering the long-term dangers. The immediate gratification outweighs future consequences.
- Sensation-Seeking: The ADHD brain often seeks novelty and excitement. Substances provide an intense, temporary rush that satisfies this craving, which can escalate to riskier use.
Inattention and Hyperactivity also contribute:
- Difficulty with Focus: Struggles in school or work lead to frustration and low self-esteem, making substances a tempting escape.
- Restlessness and Internal Chaos: The constant internal “noise” of ADHD is exhausting. Some use substances to quiet the mind or calm the body.
These issues support the self-medication hypothesis, which suggests people with ADHD use substances to alleviate their symptoms. For instance, some use stimulants like cocaine to mimic the focus-enhancing effects of ADHD medication, while others use marijuana to calm hyperactivity. This is a dangerous cycle that worsens both ADHD and addiction. For a deeper dive, see studies like “The Complicated Relationship Between ADHD and SUD“. If you’re facing this dual challenge, integrated treatment is vital. You can explore co-occurring disorder treatment options to find comprehensive support.
Shared Neurobiology and Genetic Factors
Brain structure and function also link ADHD and substance use. At the core is the dopamine reward pathway. In ADHD, impaired dopamine transmission can lead to:
- Impaired Impulse Control: The prefrontal cortex, which manages executive functions, is less effective, making it harder to resist urges like substance use.
- Reward Deficits: The ADHD brain may feel less satisfaction from normal activities. Substances provide an intense dopamine surge that compensates for this deficit, creating a powerful loop of dependence.
Genetic predisposition is also significant. Both ADHD and SUDs run in families, suggesting shared genetic vulnerabilities. Studies show genetics and environment account for up to 76% of ADHD propensity and about half of addiction risk. This means a family history of either condition increases biological susceptibility.
Psychosocial and Environmental Pressures
Daily life challenges can catalyze substance use in individuals with ADHD.
- Academic and Social Struggles: Underachievement and social rejection can lead to frustration, low self-esteem, and a desire to fit in with peer groups where substance use is common.
- Low Self-Esteem and Family Conflict: A history of personal struggles can erode self-confidence, while family stress can create an alienating environment. Substances may seem like a way to boost mood or cope.
- Maladaptive Coping: Substance use becomes a destructive way to deal with stress, boredom, and the internal chaos of ADHD.
These external pressures, combined with internal vulnerabilities, amplify the risk. Recognizing these factors is the first step toward building resilience. If you feel overwhelmed, please get confidential help now. Our compassionate advisors are here to guide you.
The Medication Debate: Does Stimulant Treatment Increase or Decrease Risk?
A common concern for those considering ADHD treatment is whether stimulant medication increases substance abuse risk. Many fear it could be a “gateway” to addiction. However, evidence-based information provides significant clarity and relief on this topic.
Debunking the “Gateway Drug” Myth
The idea that ADHD medication is a “gateway drug” has been largely debunked by extensive research.
Here’s what the science shows:
- No Increased Risk: A 2013 meta-analysis of 15 long-term studies found no link between using ADHD medication (like Ritalin) and a higher risk of future substance abuse.
- Therapeutic vs. Recreational Use: Taking medication as prescribed is fundamentally different from misuse. Therapeutic use normalizes brain function and improves focus. Recreational use involves high, non-prescribed doses and carries significant risks.
- How Stimulants Work: ADHD stimulants increase dopamine and norepinephrine in the prefrontal cortex, improving attention and impulse control. This helps regulate behavior and decision-making.
A 2016 analysis of Medicaid data involving 150,000 young people with ADHD found that those on medication were 7.3% less likely to develop an SUD than their unmedicated peers. This suggests effective ADHD treatment is protective.
How Proper Treatment for ADHD and Substance Use Can Be Protective
Proper, consistent ADHD treatment is a significant protective factor against SUDs. When symptoms are managed, the impulse to self-medicate decreases.
Effective ADHD treatment leads to:
- Reduced Impulsivity: Improved self-regulation helps individuals pause and consider consequences before acting on urges.
- Improved Academic/Work Performance: Better focus leads to success, boosting self-esteem and reducing the frustration that can drive substance use.
- Better Life Outcomes: Managing ADHD improves social relationships and personal goal achievement, which are strong deterrents to substance abuse.
- Lower SUD Likelihood: As noted, medicated individuals have a 7.3% lower risk of developing an SUD.
- Reduced Criminality: A large Swedish study found that pharmacological treatment for ADHD significantly reduced drug-related crime rates.
Furthermore, studies show that stimulant-treated adolescents have a lower risk of starting to smoke or developing an SUD compared to untreated youth. If you’re looking for support in navigating addiction, we encourage you to learn more about addiction treatment.
The Critical Role of Timing and Duration
When treatment begins and how long it continues are critical factors in reducing substance use risk.
Research highlights the following:
- Early Treatment is Protective: Starting stimulant therapy before age 10 and continuing it long-term is associated with a lower risk of substance misuse.
- Short-Term Treatment is a Risk Factor: Treatment lasting less than a year is linked to a higher likelihood of misusing cocaine, methamphetamine, or prescription stimulants.
- Late Initiation Increases Risk: Starting stimulant therapy after age 15, especially for a short duration, is associated with a 2 to 4 times higher risk of prescription stimulant misuse.
These findings, detailed in studies like “Is age of onset and duration of stimulant therapy for ADHD associated with cocaine, methamphetamine, and prescription stimulant misuse?“, underscore the need for prompt and sustained ADHD treatment. Delaying or inconsistent treatment can increase risks, making long-term management a powerful prevention strategy.
Common Substances and Compounding Factors
Individuals with ADHD are at a higher risk for substance use, but certain substances are more common, and co-occurring mental health conditions can escalate this risk. Understanding these vulnerabilities is key to prevention and intervention.

Specific Substances of Concern for ADHD and Substance Use
Teenagers and young adults with ADHD often turn to specific substances to self-medicate their symptoms.
- Alcohol: People with ADHD are nearly twice as likely to develop an alcohol use disorder, using it to quiet a restless mind or reduce social anxiety.
- Nicotine: Individuals with ADHD are twice as likely to smoke and three times more likely to become addicted. Nicotine offers a temporary boost in focus and calm.
- Marijuana: Adolescents with ADHD are 1.5 times more likely to have a cannabis use disorder. It may be used to calm hyperactivity, but it can also worsen attention and organization.
- Cocaine: Those with ADHD are almost twice as likely to develop a cocaine use disorder. Cocaine can have a paradoxical, focus-enhancing effect that mimics stimulants, leading to severe addiction.
- Prescription Stimulant Misuse: Misusing stimulants (without a prescription or in high doses) is a concern, especially among college students. The risk is higher for those who start ADHD treatment late (after age 15) and for a short duration.
These substances offer a quick but harmful way to manage ADHD symptoms, with their reinforcing effects leading to rapid dependence.
The Impact of Co-Occurring Disorders
The link between ADHD and substance use is complicated by co-occurring mental health conditions, which are common in people with ADHD. These dual diagnoses amplify substance abuse risk.
Common co-occurring disorders include:
- Anxiety and Depression: Feelings of hopelessness, worry, and sadness from these conditions are powerful triggers for self-medication.
- Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD): These are strong predictors of SUD. The SUD risk is twice as high for people with ADHD alone, but four times as high for those with both ADHD and CD, which involves defiant and antisocial behavior.
This “dual diagnosis” creates a vicious cycle where symptoms of each disorder worsen the other. This leads to:
- Worsened Outcomes: Higher risk for suicide attempts, hospitalizations, and polysubstance use.
- Treatment Complexity: Effective treatment must be integrated, addressing all conditions simultaneously. Ignoring one disorder while treating another is rarely successful.
If you are facing the challenges of co-occurring disorders, help is available. Get confidential help now to explore integrated treatment options designed for these complex needs.
Finding a Path Forward: Effective Treatment and Support
While the link between ADHD and substance use is risky, it is not a predetermined fate. With the right strategies and professional care, individuals can manage both conditions and achieve lasting recovery. Integrated treatment and proactive prevention are key.
Integrated Treatment for Dual Diagnosis
The most effective method for co-occurring ADHD and SUD is integrated treatment, which addresses both conditions simultaneously. A coordinated strategy is essential, as symptoms can overlap and mask each other.
Key components include:
- Cognitive Behavioral Therapy (CBT): A cornerstone for both conditions, Cognitive Behavioral Therapy helps change negative thought patterns and behaviors, teaching coping skills for impulsivity and cravings.
- Pharmacotherapy (Medication Management): Careful medication management is vital. This may involve controlled use of stimulants to manage ADHD symptoms and reduce the drive to self-medicate, or non-stimulants like atomoxetine, which have lower abuse potential.
- Motivational Interviewing (MI): This therapy strengthens an individual’s motivation to change by resolving ambivalence about treatment.
- Family Therapy: Involving family is crucial for adolescents. It improves communication and creates a supportive home environment. SoberSteps offers resources for various Therapy options, including Group Therapy and Individual Therapy for Addiction.
- Specialized Approach: Finding providers experienced in dual diagnosis is critical. These programs tailor treatment to complex, individual needs.
No one should face these challenges alone. We invite you to explore co-occurring disorder treatment options through SoberSteps.
Prevention Strategies for Parents and Caregivers
Parents and caregivers play an invaluable role in mitigating substance abuse risks for adolescents with ADHD. Proactive strategies can make a significant difference.
- Open Communication: Create a nonjudgmental space to talk about substance use and the specific dangers for someone with ADHD.
- Educate on Risks: Teach your child about commonly misused substances and why they are ultimately harmful.
- Monitor Behavior: Stay involved in your child’s life. Know their friends and be aware of changes in mood or behavior.
- Promote Healthy Coping Skills: Help your child find constructive ways to manage stress and emotions, such as hobbies, exercise, or mindfulness.
- Ensure Consistent ADHD Treatment: Work with professionals to maintain consistent and appropriate treatment, as this is a key protective factor.
- Build Self-Esteem: Celebrate your child’s strengths and successes to counteract feelings of inadequacy.
- Set Clear Boundaries: Establish and enforce clear rules and consequences regarding substance use.
- Seek Professional Guidance: Use family therapy or other Behavioral Health Support to resolve conflicts and improve family dynamics.
Long-Term Consequences of Untreated ADHD and Substance Use
Untreated co-occurring ADHD and substance use disorders can lead to severe, lasting negative consequences.
Individuals with both conditions face:
- Increased Hospitalization and Suicide Risk: Impulsivity and emotional distress from both disorders significantly increase the risk of crises, accidents, and suicide attempts.
- Chronic Instability: Difficulties maintaining employment and financial hardship are common.
- Legal Problems: Impulsive and substance-seeking behaviors can lead to arrests and incarceration.
- Damaged Relationships: Symptoms can strain family and social bonds, leading to isolation.
- Poorer Health: Chronic substance abuse takes a heavy toll on physical and mental health, and the conditions can become more severe and difficult to treat.
These consequences show why early, comprehensive treatment is life-saving. Addressing both conditions can change an individual’s life trajectory. We offer various Levels of Care, including Inpatient Drug Rehab and Intensive Outpatient programs, to meet diverse needs.
Conclusion
The connection between ADHD and substance use is undeniable and complex. We’ve explored how the core symptoms of ADHD, shared neurobiological vulnerabilities, and psychosocial pressures can lift the risk of developing a substance use disorder. We’ve also debunked the myth that ADHD medication increases this risk, showing instead that proper, early, and consistent treatment can be a powerful protective factor.
The good news is that this doesn’t have to be a risky business without hope. With understanding comes empowerment. Untreated ADHD is the major risk factor for substance use issues, not the treatment itself. By recognizing the signs, seeking a proper diagnosis, and engaging in integrated treatment that addresses both ADHD and any co-occurring substance use disorders, individuals can find a path to stability and recovery.
At SoberSteps, we believe in empowering you with knowledge and connecting you with the support you need. Taking that first step toward understanding and seeking help is crucial. If you or a loved one are navigating the challenges of ADHD and substance use, please don’t hesitate to reach out. We provide a confidential helpline to explore treatment options and guide you toward a healthier future.
Get confidential help now. Your journey to recovery and well-being starts here.