
Addiction Help: Your First Steps to Recovery
Ready to get help addiction? Find signs, treatment options, and support with SoberSteps. Start your confidential recovery journey today.
Benzodiazepines Addiction is a growing crisis affecting millions who started with a legitimate prescription. These medications—prescribed for anxiety, insomnia, or seizures—can trap users in a cycle of dependence that’s difficult to escape without professional help.
What You Need to Know About Benzodiazepines Addiction:
Many people don’t realize they’re becoming dependent until it’s too late. What starts as a doctor’s solution can become a “benzo trap”—a situation where stopping the medication feels impossible due to severe withdrawal.
The path from prescription to addiction often begins with a legitimate prescription, but tolerance builds quickly (often within 4 weeks). Physical dependence follows, and the user continues taking the medication simply to avoid severe withdrawal symptoms, not for the original benefit.
Research shows that 33.2% of people who use benzodiazepines transition to long-term use, increasing their risk of addiction. Even more concerning, approximately 80% of benzodiazepine abuse involves other substances, particularly opioids and alcohol, which dramatically increases the risk of fatal overdose.
At Sober Steps, we’ve helped countless individuals steer the complexities of Benzodiazepines Addiction through education, community support, and access to confidential treatment options. Our mission is to provide you with the knowledge and resources you need to break free from dependence and reclaim your life.
It is easy to assume that a medication prescribed by a doctor is inherently safe. However, the very effectiveness of benzodiazepines can pave the way for dependence and, ultimately, Benzodiazepines Addiction. Understanding this path is the first step toward prevention or recovery.
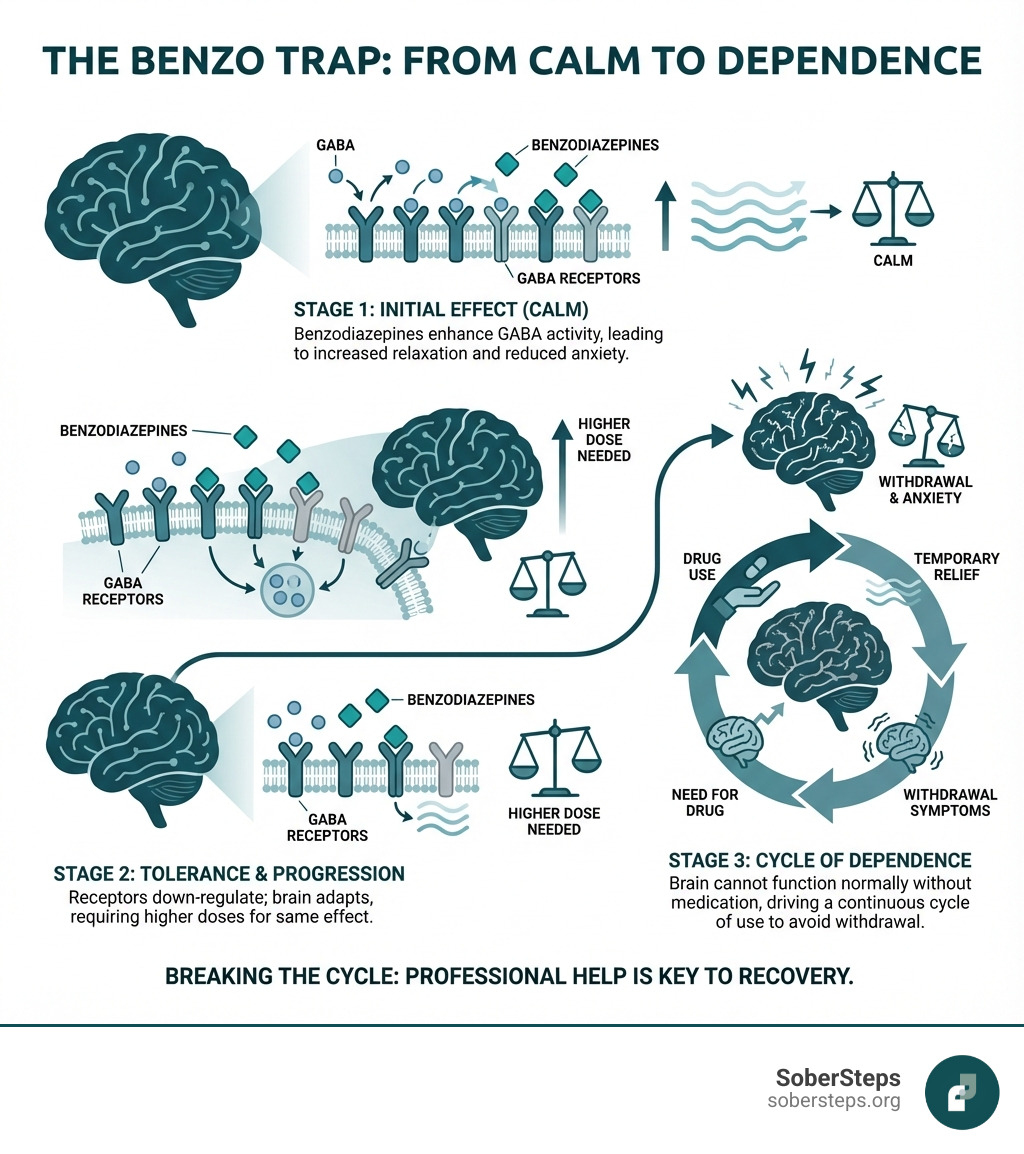
When you take a benzodiazepine, your brain’s chemistry shifts, bringing a sense of calm. Over time, your brain adapts to this new chemical environment and its own calming systems become less effective. This adaptation leads to tolerance, where you need more of the drug to get the same effect. From there, physical dependence can quickly develop, making it incredibly difficult to stop without experiencing dangerous withdrawal symptoms.
Statistics paint a clear picture: a significant 33.2% of individuals who start using benzodiazepines will transition to long-term use. This drastically increases the risk of developing a full-blown Benzodiazepines Addiction.
To grasp how Benzodiazepines Addiction takes hold, we need to look at the brain. Benzodiazepines boost the effects of GABA, your brain’s natural “brake pedal,” which slows down brain activity and produces a calming effect. With constant exposure, your brain adapts by reducing its sensitivity to GABA. This is the core mechanism behind tolerance: the original dose becomes less effective, prompting you to take more to achieve the same relief. For a deeper dive, you can read this scientific research on benzodiazepine tolerance.
As tolerance increases, so does the risk of physical dependence. Your brain becomes so accustomed to the drug that it struggles to function without it, triggering withdrawal symptoms if you try to stop. Short-acting benzodiazepines like Xanax can lead to quicker dependence due to more pronounced “inter-dose withdrawal,” where anxiety returns between doses. This can lead to taking the next dose sooner or in higher amounts.
Psychological dependence can develop alongside physical dependence. You may begin to feel that you cannot cope with daily life, stressful situations, or sleep without the medication, even when safer strategies could help. Together, these processes can pull you deeper into the benzo trap.
Recognizing the signs of Benzodiazepines Addiction is crucial. It often begins with a legitimate prescription and the signs can be subtle at first.
If you or someone you know exhibits several of these signs, it is a strong indicator that professional help is warranted.
While anyone can develop a dependence on benzodiazepines, certain factors significantly increase the risk of Benzodiazepines Addiction.
The allure of quick relief can make benzodiazepines seem like a miracle drug, but the reality of Benzodiazepines Addiction comes with significant dangers. Long-term abuse and the severe withdrawal process pose serious, sometimes life-threatening, health risks.
One of the most immediate dangers is the risk of overdose, especially when benzodiazepines are combined with other substances. Understanding the full scope of these dangers is paramount.
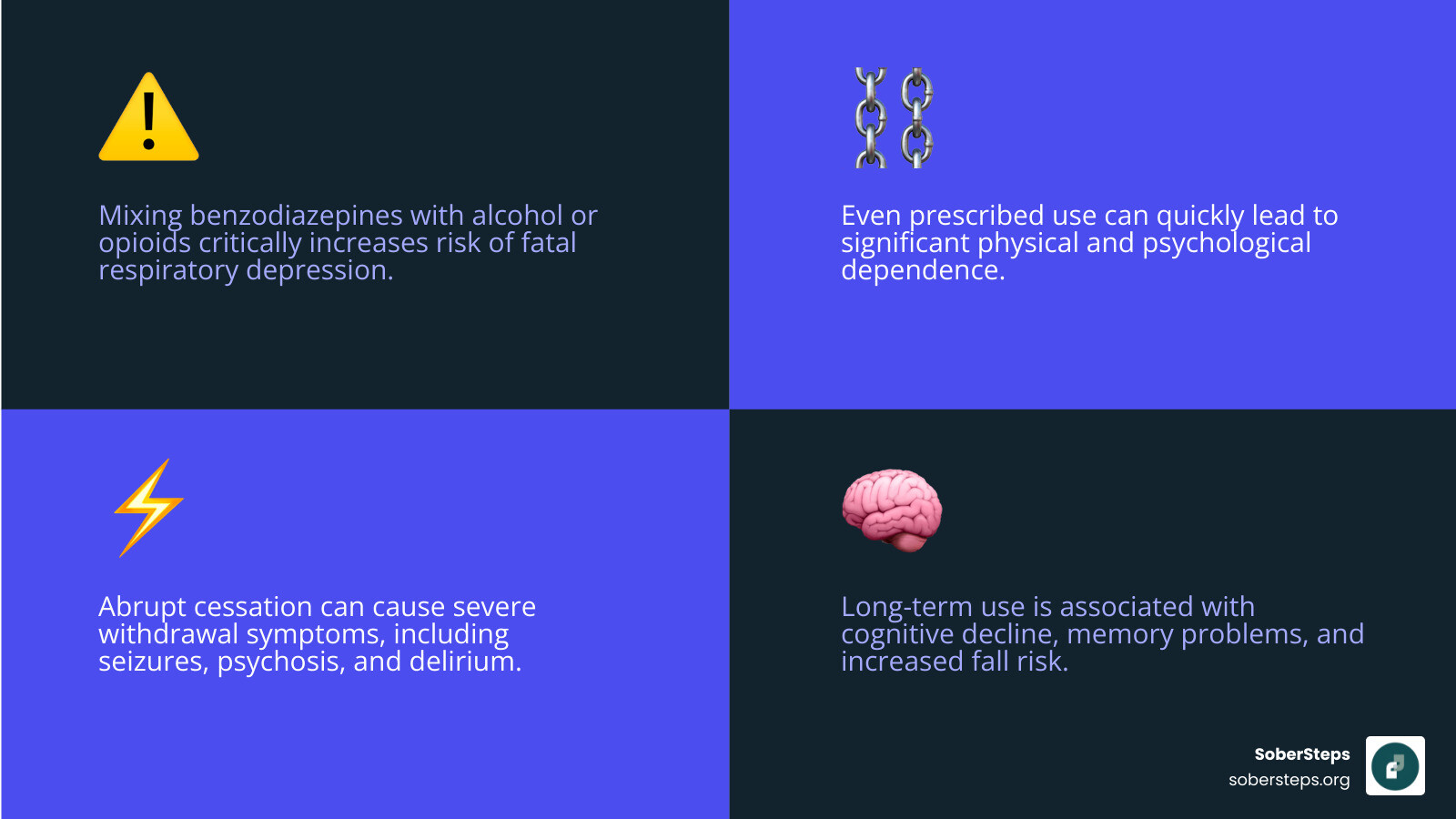
Stopping benzodiazepines “cold turkey” after developing dependence is extremely dangerous and can be fatal. This is why medical supervision is absolutely critical during detox from Benzodiazepines Addiction.
When someone abruptly stops, their brain loses its “brake pedal,” leading to a surge of uncontrolled neurological activity known as Benzodiazepine Withdrawal Syndrome.
The withdrawal timeline varies based on the specific benzodiazepine, dose, and length of use. Short-acting benzos often produce withdrawal symptoms within hours to a couple of days, while long-acting benzos may have a delayed onset. Symptoms can peak within the first one to two weeks and then gradually lessen, though some psychological and sleep-related issues can linger. Regardless of the specifics, medical detox is the only safe approach.
Beyond withdrawal, prolonged use of benzodiazepines, even as prescribed, can lead to a host of long-term side effects. This is a critical aspect of understanding Benzodiazepines Addiction.
The American Academy of Family Physicians (AAFP) provides valuable addiction and side effects information, highlighting why these drugs are meant for short-term use only.
The dangers of Benzodiazepines Addiction are compounded when other substances are involved, which is alarmingly common. Approximately 80% of benzodiazepine abuse involves other drugs.
Certain populations also face heightened risks:
The journey through Benzodiazepines Addiction can feel isolating, but hope for recovery is always present. With professional help, individuals can break free from the “benzo trap.” The prognosis for recovery is positive for those who commit to a structured treatment plan.
At Sober Steps, we believe in the power of supportive care and have seen countless individuals successfully steer this path.
Diagnosing Benzodiazepines Addiction, formally known as Sedative, Hypnotic, or Anxiolytic Use Disorder, requires a comprehensive evaluation by a healthcare professional. The diagnosis is not just about taking the drug, but about the pattern of use and its negative impact on a person’s life.
Clinicians use criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). A diagnosis is considered if a person’s benzodiazepine use leads to significant impairment or distress. Key indicators include:
The diagnostic process involves a medical evaluation, a detailed history of substance use and mental health, and sometimes screening questionnaires. Being honest with providers is crucial for an accurate diagnosis and effective treatment plan.
For Benzodiazepines Addiction, medical detox is a life-saving necessity. Stopping “cold turkey” can cause fatal withdrawal symptoms like seizures. Professional medical supervision is paramount.
Medical detox almost always involves a medically supervised taper, where the dosage is gradually reduced over weeks or months. This allows the brain to slowly re-adjust, minimizing the severity of withdrawal. Key aspects include:
Medical detox is the essential first step that provides a safe foundation for therapy.
Detox is just the beginning. Lasting recovery from Benzodiazepines Addiction requires a comprehensive approach that addresses the root causes of dependence.
Recovery is a personal journey, and the best treatment plan is always customized to the individual’s needs. Sober Steps can help you explore options privately, so you can find care that matches your circumstances and comfort level.
While benzodiazepines can offer short-term relief, their potential for addiction highlights the importance of prevention and exploring safer alternatives. Our goal is to empower individuals with knowledge to make informed decisions about their health.
This involves open communication between doctors and patients and a willingness to consider non-pharmacological approaches first.
Preventing Benzodiazepines Addiction starts with responsible prescribing and informed patient choices. These steps can significantly reduce the risk of dependence:
By following these guidelines, we can minimize the impact of Benzodiazepines Addiction.
For many conditions treated with benzodiazepines, there are numerous safer, non-addictive alternatives that can prevent Benzodiazepines Addiction altogether.
| Feature | Benzodiazepines | Safer Alternatives (SSRIs, Buspirone, Therapy, Lifestyle) |
|---|---|---|
| Primary Action | Fast-acting relief for acute anxiety/insomnia | Address underlying causes; slower onset, sustained relief |
| Addiction Potential | High, especially with long-term use | Very low to none |
| Withdrawal Symptoms | Severe, potentially life-threatening | Generally mild or none |
| Long-Term Side Effects | Cognitive impairment, increased fall risk, dementia link | Generally fewer, different side effect profiles |
| Mechanism | Improves GABA (immediate calming) | Modulates serotonin/norepinephrine; teaches coping skills |
Non-Addictive Medications:
Therapies:
Lifestyle Changes:
Herbal Supplements:
Some people find relief from remedies like valerian root or chamomile. However, these are not regulated like prescription medications, and they can interact with other drugs. Always consult a healthcare professional before trying any supplement, particularly if you are already taking benzodiazepines or other medications.
We have explored the complex world of Benzodiazepines Addiction, from how these medications work and lead to dependence, to the serious dangers of withdrawal and long-term use. We have also highlighted the critical steps for diagnosis, the necessity of medical detox, and the comprehensive treatment approaches that offer a pathway to healing.
The journey out of the “benzo trap” may seem daunting, but recovery is not just a possibility—it is a reality for countless individuals. With the right support, guidance, and commitment, you can break free from the cycle of dependence and reclaim a life of health and well-being.
Recovery is a journey, not a destination. It involves understanding, patience, and a willingness to seek help. At Sober Steps, we are committed to being a confidential, anonymous online resource, connecting individuals across the United States and its territories to mental health and substance use disorder treatment. Our mission is to provide you with the tools and connections you need to steer this journey with confidence and privacy.
If you or a loved one is struggling with Benzodiazepines Addiction, please know that you do not have to face it alone. Help is available, and a brighter, substance-free future is within reach. Take the courageous first step today by exploring treatment options that respect your need for safety and anonymity.
Find a treatment program near you and begin your journey to recovery today.

Ready to get help addiction? Find signs, treatment options, and support with SoberSteps. Start your confidential recovery journey today.
Find support & healing with comprehensive resources for families facing addiction. SoberSteps guides you from crisis to calm. Get help now!

Discover how nutrition in recovery heals your body & mind, reduces cravings, and strengthens your sobriety. Start your healthy journey today!
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.