Understanding Drug Withdrawal: Your First Step to Recovery
Drug Withdrawal is the set of physical and mental symptoms that occur when someone who is dependent on a substance reduces or stops using it. It happens because the body has adapted to the drug’s presence and struggles to function normally without it.
Quick Facts About Drug Withdrawal:
- What causes it: Physical dependence develops when your brain and body adjust to regular substance use
- Common symptoms: Anxiety, nausea, sweating, tremors, insomnia, muscle aches, and intense cravings
- Timeline: Varies by substance—alcohol (6-24 hours onset), opioids (8-24 hours), benzodiazepines (1-4 days)
- Can it be dangerous? Yes—withdrawal from alcohol and benzodiazepines can be life-threatening without medical supervision
- Treatment: Medically supervised detox is the safest approach; call (844) 491-5566 for confidential support 24/7
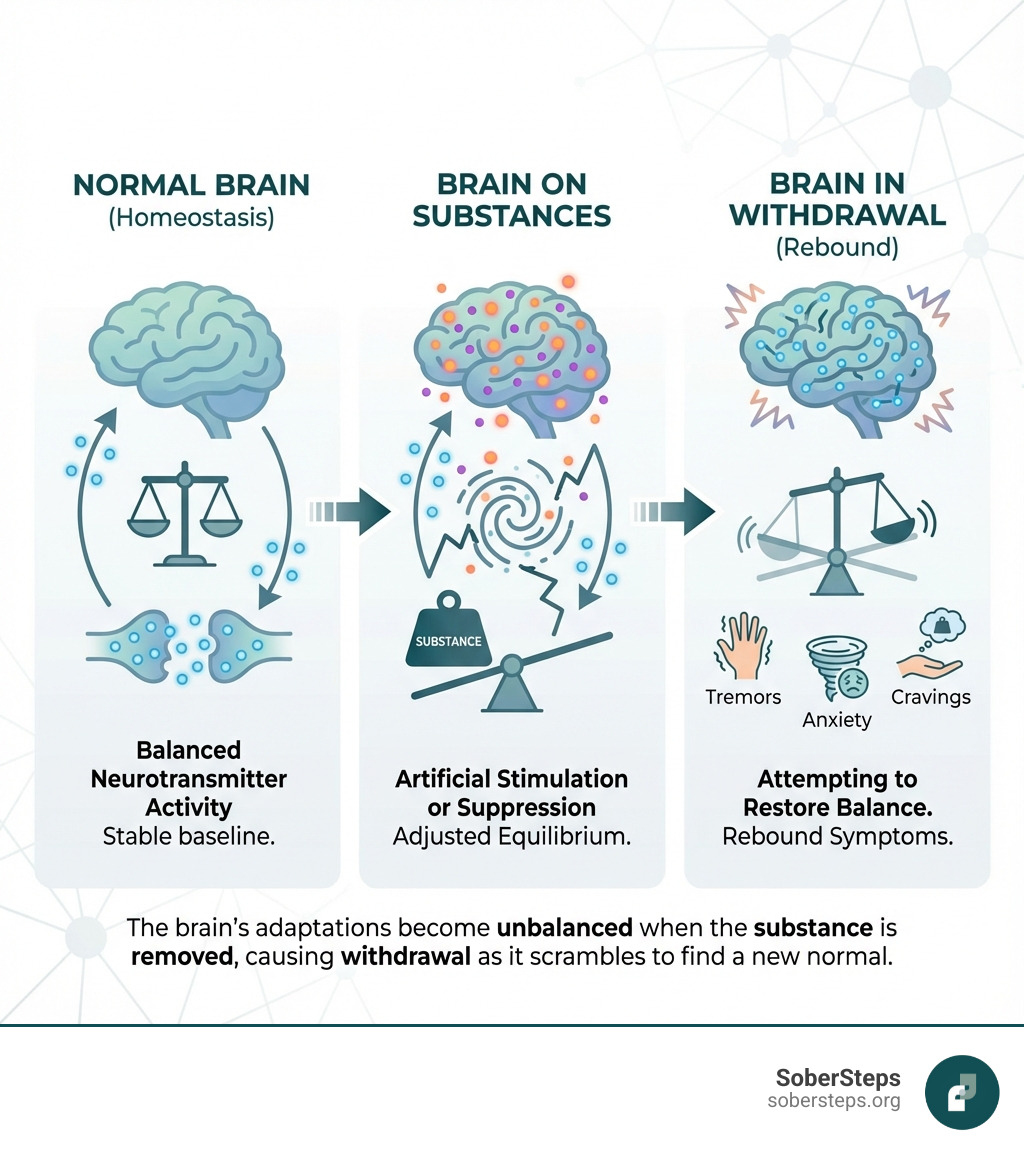
Withdrawal occurs because your body seeks homeostasis—a state of balance. When you use substances regularly, your brain chemistry changes to compensate for the drug’s effects. It adjusts neurotransmitter levels and receptor sensitivity to maintain equilibrium. When the substance is suddenly removed, these adaptations become unbalanced, causing withdrawal symptoms as your body scrambles to find its new normal.
It’s crucial to understand: Physical dependence is not the same as addiction. You can be physically dependent on a medication prescribed by your doctor and experience withdrawal if you stop taking it suddenly. Addiction involves compulsive use despite harmful consequences. However, both conditions require professional guidance to manage safely.
The dangers of withdrawal are real. Severe alcohol withdrawal can lead to delirium tremens (DTs), which is fatal in about 15% of untreated cases. Benzodiazepine withdrawal can cause life-threatening seizures. Even opioid withdrawal, while rarely fatal, is so uncomfortable that it drives many people back to using—often resulting in overdose due to reduced tolerance.
This is why professional help matters. You don’t have to suffer through withdrawal alone, and you shouldn’t try to “tough it out” at home. Medical supervision ensures your safety, eases your discomfort, and dramatically increases your chances of successful recovery. If you or someone you love is struggling with substance dependence, confidential help is available right now at (844) 491-5566.
At Sober Steps, we’ve dedicated ourselves to helping individuals steer the complexities of Drug Withdrawal and recovery by connecting them with appropriate treatment resources and evidence-based information. We understand that taking the first step can feel overwhelming, but you’re not alone on this journey.
Understanding the Science of Drug Withdrawal
To truly grasp Drug Withdrawal, we need to dig a little into the fascinating, yet complex, world of our brain chemistry. When we use certain substances repeatedly, our brains and bodies begin to adapt to their constant presence. This isn’t a sign of weakness; it’s a physiological response, an attempt by our bodies to maintain a state of balance, or homeostasis.
Why does withdrawal occur? Imagine your brain as a finely tuned orchestra. Each neurotransmitter is an instrument, playing its part to create a harmonious symphony of thoughts, emotions, and bodily functions. When a drug is introduced, it’s like adding a new, powerful instrument that starts playing very loudly. Our brain, in its effort to maintain balance, might quiet down other instruments or even stop some from playing altogether, trying to compensate for the new, dominant sound.
For instance, drugs might flood the brain with dopamine, our “feel-good” neurotransmitter, or they might improve the calming effects of GABA. Over time, the brain becomes accustomed to this altered state. When the drug is removed, that powerful new instrument suddenly goes silent. The other instruments, which had been quieted or stopped, can’t immediately ramp back up to their normal levels. This creates a “rebound” effect, a cacophony of unbalanced brain chemistry, leading to the uncomfortable and often distressing symptoms we associate with withdrawal.
This intricate dance of adaptation is a core concept in the neurobiology of addiction. The brain essentially reorganizes itself at a cellular level to accommodate the drug, making the absence of the substance a profound shock to the system.
Physical vs. Psychological Dependence
When we talk about dependence, it’s important to distinguish between its physical and psychological aspects.
Physical dependence is a physiological adaptation where our bodies become so accustomed to a substance that they require it to function “normally.” If the substance is removed, our bodies react with somatic (physical) symptoms. These can range from nausea, vomiting, sweating, and tremors to more severe reactions like seizures and delirium tremens. This is the body’s way of protesting the sudden absence of something it has integrated into its daily operations. Tolerance, where we need more of a substance to achieve the same effect, is often a precursor to physical dependence.
Psychological dependence, on the other hand, is characterized by emotional and motivational withdrawal symptoms. These affect our cognitive functioning and emotional state. Symptoms often include intense cravings, anxiety, anhedonia (the inability to feel pleasure), agitation, depression, and irritability. While physical symptoms can be severe, the psychological aspects of withdrawal can be equally, if not more, challenging, driving individuals back to substance use despite their desire to quit. Withdrawal symptoms can even occur without physical dependence, particularly in behavioral addictions, where the brain’s reward pathways are heavily involved.
Factors Influencing Withdrawal Severity
The journey through Drug Withdrawal is highly individualized. What one person experiences can be vastly different from another, even when withdrawing from the same substance. Several key factors play a role in influencing the severity and duration of withdrawal symptoms:
- Type of Substance: Some drugs, like alcohol and benzodiazepines, have potentially life-threatening withdrawal symptoms. Others, like opioids, produce uncomfortable but rarely fatal symptoms. Stimulant withdrawal, while not typically life-threatening, can be profoundly distressing psychologically.
- Duration and Amount of Use: Generally, the longer someone has used a substance and the higher the doses they’ve taken, the more severe their withdrawal symptoms are likely to be. The body has had more time to adapt and will have a harder time readapting to the substance’s absence.
- Individual Health Factors: A person’s overall physical and mental health significantly impacts their withdrawal experience. Age, pre-existing medical conditions, nutritional status, and even genetics can influence symptom severity. For example, some individuals have genetic predispositions that affect how they experience alcohol and nicotine withdrawal. Co-occurring mental health conditions, such as depression or anxiety, can also exacerbate withdrawal symptoms and make the process more challenging.
- Method of Administration: While not always explicitly detailed in research, how a drug is administered (e.g., intravenously, smoked, orally) can sometimes affect the speed of onset and intensity of withdrawal, as it impacts how quickly the substance enters and leaves the body.
Understanding these variables helps us appreciate why a personalized approach to withdrawal management is so crucial.
Symptoms and Timelines for Common Substances
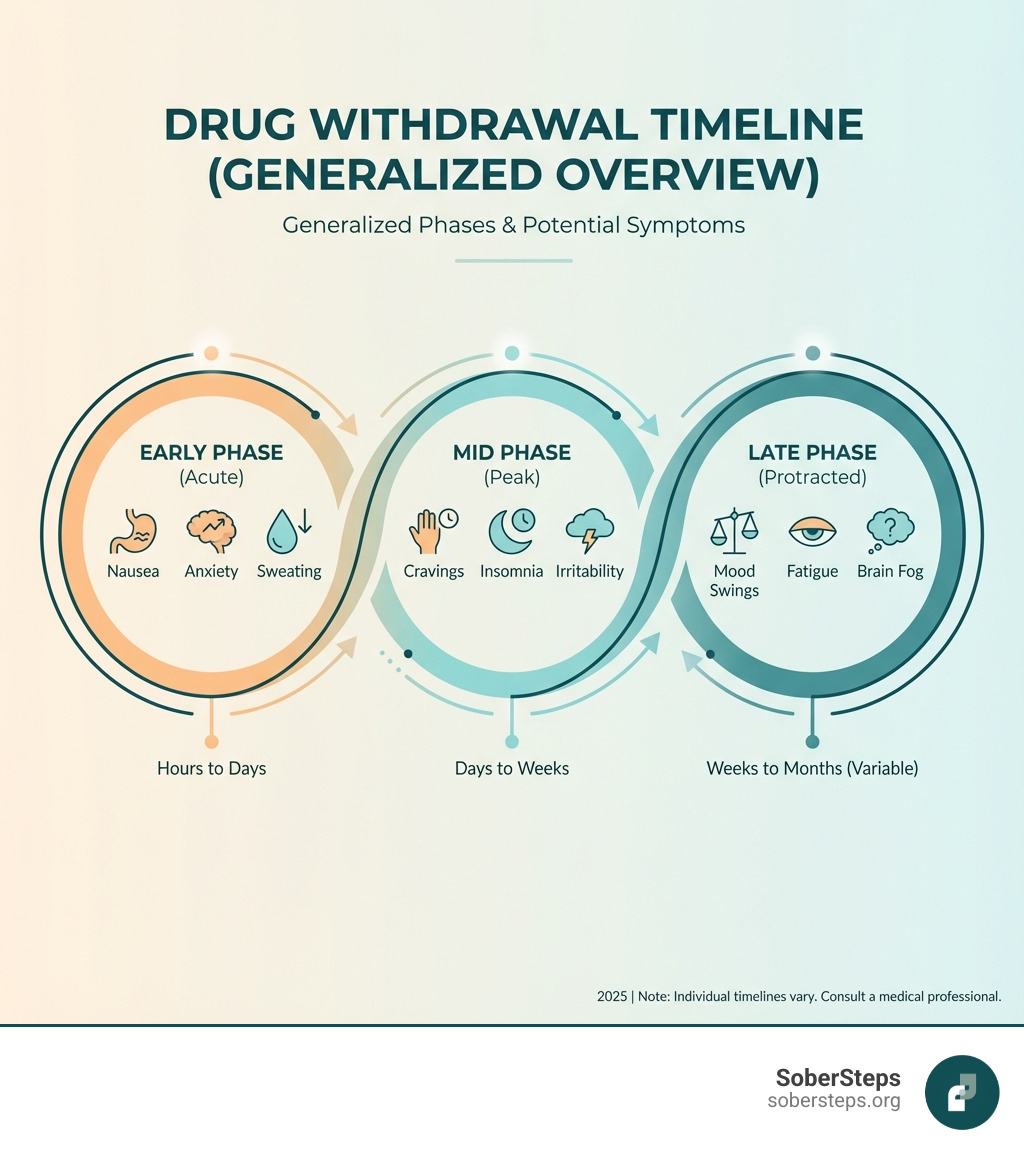
The spectrum of Drug Withdrawal symptoms is broad, varying significantly based on the substance involved. Let’s explore some common substances and their typical withdrawal experiences.
Alcohol Withdrawal Symptoms and Timeline
Alcohol withdrawal can be one of the most dangerous and potentially lethal forms of withdrawal. When someone who is physically dependent on alcohol suddenly stops drinking, their central nervous system, which has been suppressed by alcohol, goes into overdrive.
Symptoms can begin as early as 6-24 hours after the last drink and typically include:
- Anxiety and agitation
- Shakes (tremors), especially in the hands
- Nausea and vomiting
- Headaches
- Profuse sweating
- Increased heart rate and blood pressure
- Insomnia
The most severe symptoms usually peak between 36-72 hours. These can include hallucinations (alcoholic hallucinosis) and seizures, which are serious medical emergencies. A particularly severe and life-threatening complication is Delirium Tremens (DTs), characterized by extreme confusion, disorientation, severe agitation, fever, and intense hallucinations. DTs occur in fewer than 5% of people experiencing alcohol withdrawal, but if left untreated, it can be fatal in about 15% of those cases. The entire withdrawal process usually lasts 2-10 days.
Given these risks, medically supervised detox is absolutely essential for alcohol withdrawal. For more in-depth information on managing alcohol withdrawal, we encourage you to explore our detailed guide. If you or a loved one needs safe alcohol detox guidance, please call (844) 491-5566 for confidential support.
| Substance | Onset of Withdrawal Symptoms | Peak Severity of Symptoms | Typical Duration of Acute Withdrawal |
|---|---|---|---|
| Alcohol | 6-24 hours | 36-72 hours | 2-10 days |
| Short-Acting Opioids | 8-24 hours | Early in duration | 4-10 days |
| Long-Acting Opioids | 2-4 days (up to 48 hours) | Not explicitly defined | 10-20 days |
| Short-Acting Benzodiazepines | 1-2 days | First 2 weeks | 2-4 weeks or longer |
| Long-Acting Benzodiazepines | 2-7 days | First 2 weeks | 2-8 weeks or longer |
Opioid (Heroin, Fentanyl, Painkillers) Withdrawal
Opioid withdrawal, though rarely fatal, is notoriously unpleasant and can feel like the worst flu imaginable. It’s often described as uncomfortable, driving many individuals back to using to escape the misery.
Symptoms typically begin within 8-24 hours for short-acting opioids (like heroin or some prescription painkillers) and can last 4-10 days. For longer-acting opioids (such as methadone), symptoms might take 2-4 days to emerge and can last 10-20 days.
Common symptoms include:
- Flu-like symptoms: Runny nose, watery eyes, yawning, sneezing
- Muscle and bone pain
- Abdominal cramps, nausea, vomiting, and diarrhea
- Insomnia and restless sleep
- Cold flashes with goosebumps (“cold turkey” sensation)
- Uncontrollable leg movements
- Anxiety and agitation
- Intense cravings
The severe discomfort of opioid withdrawal, combined with the intense cravings, poses a high risk of relapse. If someone relapses after a period of abstinence, their tolerance will have decreased, significantly increasing the risk of an accidental overdose. For more comprehensive information, you can refer to Opiate and opioid withdrawal information.
Benzodiazepine (Xanax, Valium) Withdrawal
Benzodiazepines, often prescribed for anxiety and sleep disorders, can lead to severe and potentially life-threatening withdrawal if stopped abruptly. This is because they work by enhancing the calming effects of the GABA neurotransmitter. When removed, the brain experiences a profound rebound hyperexcitability.
Withdrawal symptoms can begin 1-4 days after the last use, peaking in severity within the first two weeks. They can include:
- High anxiety, panic attacks, and extreme agitation
- Insomnia and nightmares
- Tremors and muscle aches
- Nausea, vomiting, and headaches
- Heart palpitations
- Memory problems and poor concentration
- Seizures, which are a significant risk and can be fatal.
A challenging aspect of benzodiazepine withdrawal is the potential for Protracted Withdrawal Syndrome (PAWS), where certain symptoms can persist for months or even years after acute withdrawal, including anxiety, insomnia, and cognitive difficulties. Due to the serious risks, gradual tapering under strict medical supervision is the safest and most effective way to withdraw from benzodiazepines. For help with benzodiazepine dependence, call our 24/7 helpline at (844) 491-5566.
Stimulant (Cocaine, Meth, Adderall) Withdrawal
Withdrawal from stimulants like cocaine, methamphetamine, and Adderall is generally not considered physically dangerous, but it can be uncomfortable and psychologically distressing. The term “withdrawal syndrome” isn’t always strictly applied, as it’s often referred to as a “post-toxicity syndrome” or a “crash.”
Symptoms typically begin within 24 hours of last use and can last 3-5 days. They are primarily psychological and include:
- The “crash”: A period of extreme fatigue and lethargy, often accompanied by a profound lack of motivation.
- Intense depression and anhedonia (inability to experience pleasure)
- Increased appetite
- Excessive sleep or insomnia
- Agitation and irritability
- Difficulty concentrating
- Paranoia
While the physical risks are low, the severe depression and anhedonia can significantly increase the risk of suicidal thoughts and relapse. Supportive care and behavioral management are crucial during this period.
How to Safely Manage Withdrawal

Navigating Drug Withdrawal safely is paramount, not just for comfort but often for survival. The idea of “cold turkey” might sound tough and determined, but it can be incredibly dangerous, even fatal, for certain substances. We strongly advocate for professional help, as it provides the safety net and expertise needed during this critical time.
The Importance of Medically Supervised Drug Withdrawal
Attempting to stop using substances like alcohol or benzodiazepines abruptly and without medical oversight can lead to severe and life-threatening complications. This is why “cold turkey” is a dangerous gamble. Medically supervised detox, often referred to as withdrawal management, is designed to keep you safe and as comfortable as possible.
During medical detox, healthcare professionals:
- Monitor vital signs: Your heart rate, blood pressure, temperature, and breathing are continuously monitored to catch any dangerous fluctuations.
- Prevent complications: They are trained to recognize early signs of severe complications like seizures, delirium tremens, or severe dehydration and intervene immediately.
- Manage severe discomfort: Medications are administered to alleviate the most distressing symptoms, making the process more tolerable and reducing the likelihood of relapse.
Medical detox is not the entire journey, but it is the crucial first step on the path to recovery. It clears the substances from your body safely, setting the stage for deeper therapeutic work. To learn more about how medical detox can help you or a loved one, call (844) 491-5566.
Treatment Settings for Detoxification
The right setting for detoxification depends on several factors, including the type of substance, the severity of dependence, your overall health, and your support system. We can help you determine the most appropriate level of care.
- At-home Detox (with medical supervision): For individuals with mild to moderate dependence, a strong support system, and no significant co-occurring medical or mental health issues, at-home detox can be an option. This still requires close medical supervision, often with daily check-ins with a healthcare provider and prescribed medications to manage symptoms. It’s crucial to proceed very slowly and carefully in such cases.
- Inpatient Detox Facilities: These specialized facilities provide a structured, substance-free environment with 24/7 medical care and supervision. They are ideal for individuals with moderate to severe dependence, a history of complicated withdrawals, or those who need a higher level of support to prevent relapse during the acute withdrawal phase.
- Hospital-based Detox: For the most severe and high-risk cases, such as those with a history of seizures, delirium tremens, or significant co-occurring medical conditions, a hospital setting offers the most intensive medical care. This ensures immediate access to emergency interventions if needed.
Choosing the right level of care is a critical decision that should always be made in consultation with medical professionals.
Medications Used to Ease Drug Withdrawal
Medication-Assisted Treatment (MAT) plays a vital role in making Drug Withdrawal safer and more manageable. The Food and Drug Administration (FDA) has approved several medications to help reduce the severity of withdrawal symptoms and cravings, custom to the specific substance.
- Buprenorphine: A partial opioid agonist, buprenorphine can significantly diminish opioid withdrawal symptoms and cravings with a lower risk of misuse compared to full agonists. It can shorten the length of detox and is also used for long-term maintenance.
- Methadone: A long-acting full opioid agonist, methadone is used for both withdrawal relief and long-term maintenance for opioid dependence. It works by reducing cravings and preventing withdrawal onset by creating cross-tolerance.
- Naltrexone: An opioid antagonist, naltrexone is used after detox to prevent relapse. It blocks opioid receptors, preventing euphoric effects and reducing cravings. It’s crucial that Naltrexone is not taken while opioids are still in the system, as it can precipitate severe withdrawal.
- Benzodiazepines: For alcohol withdrawal, benzodiazepines (like diazepam or lorazepam) are the drugs of choice. They help manage severe symptoms, prevent seizures, and reduce anxiety by calming the central nervous system.
- Comfort Medications: Beyond substance-specific medications, other drugs are used to manage general discomfort. Clonidine, for example, can alleviate symptoms like anxiety, agitation, muscle aches, sweating, and runny nose, though it doesn’t address cravings directly. Other medications can target specific symptoms such as nausea, vomiting, diarrhea, and insomnia to improve comfort during detox.
These medications, used under medical guidance, are critical tools in providing effective and humane withdrawal management. For detailed clinical guidance, you can refer to Clinical guidelines for withdrawal management.
The Road to Recovery: Support and Long-Term Success
Completing detox is a monumental achievement, but it’s just the beginning of the recovery journey. The period immediately following withdrawal is often fragile, and establishing a robust support system and a comprehensive long-term treatment plan is essential for sustained sobriety. We understand that continued care is paramount to lasting success.
The Role of Counseling and Therapy
After the physical discomfort of Drug Withdrawal subsides, the psychological work begins. Counseling and therapy are critical for addressing the underlying issues that contributed to substance use and for developing healthy coping mechanisms.
- Individual Counseling: Provides a safe space to explore personal challenges, trauma, co-occurring mental health disorders, and develop personalized strategies for managing triggers and cravings.
- Cognitive Behavioral Therapy (CBT): A highly effective therapy that helps individuals identify and change negative thought patterns and behaviors that lead to substance use.
- Group Therapy: Offers a supportive environment where individuals can share experiences, learn from peers, and practice new social skills in a judgment-free setting. This sense of community and shared struggle is incredibly powerful.
Most people need long-term treatment after detox, as it’s unrealistic to expect withdrawal management alone to lead to sustained abstinence. Therapy helps address the root causes of addiction, rather than just the physical dependence.
Managing Cravings and Preventing Relapse
Cravings are a natural part of recovery and can persist long after acute withdrawal. Learning to manage them is a key skill for preventing relapse.
- Identifying Triggers: Understanding what situations, emotions, or people might provoke a craving is the first step. Once identified, strategies can be developed to avoid or steer these triggers.
- Developing Coping Strategies: This involves learning healthy alternatives to using substances when cravings arise. This could include exercise, meditation, hobbies, talking to a sponsor, or engaging in therapy techniques.
- The Difference Between a Lapse and a Relapse: A lapse (a single instance of substance use) is not the same as a full-blown relapse (returning to regular use). A lapse can be a learning opportunity if addressed quickly, without letting shame or guilt derail the entire recovery process. We help individuals understand that a lapse doesn’t mean they’ve “failed.”
An aftercare plan is crucial. This might include ongoing individual or group therapy, participation in self-help groups like Narcotics Anonymous or SMART Recovery, or even intensive outpatient treatment, all designed to provide ongoing support and structure.
How Friends and Family Can Provide Support
Supporting someone through Drug Withdrawal and early recovery can be challenging, but friends and family play a vital role.
- Educating Themselves: Learning about the specific substance, its withdrawal symptoms, and the recovery process helps loved ones understand what the individual is going through and respond effectively.
- Providing a Stable Environment: Ensuring a drug-free, calm, and supportive home environment minimizes stress and potential triggers.
- Encouraging Treatment: Actively supporting and encouraging engagement in professional treatment, counseling, and support groups is invaluable.
- Setting Boundaries: Healthy boundaries are essential for both the individual in recovery and their loved ones. This protects everyone’s well-being and fosters a healthy recovery dynamic.
- The Importance of Self-Care for Supporters: Supporting someone through this process can be emotionally taxing. It’s crucial for friends and family to prioritize their own self-care, seek their own support (e.g., Al-Anon), and ensure they have someone to talk to when things get difficult.
Frequently Asked Questions about Drug Withdrawal
Can you die from drug withdrawal?
Yes, absolutely. While some forms of Drug Withdrawal are primarily uncomfortable, others can be acutely dangerous and even fatal without proper medical intervention. Withdrawal from certain drugs, particularly alcohol and benzodiazepines, poses significant life-threatening risks. Alcohol withdrawal can lead to severe seizures and Delirium Tremens (DTs), which can be fatal in about 15% of untreated cases. Similarly, abrupt cessation of benzodiazepines can cause severe seizures and other dangerous complications. Opioid withdrawal, while rarely directly fatal, is distressing and can lead to complications like severe dehydration. More critically, the profound discomfort often drives individuals to relapse, and a reduced tolerance after abstinence dramatically increases the risk of fatal overdose.
How long does the brain take to recover from drug use?
The timeline for the brain to recover from drug use varies greatly depending on the substance, duration of use, individual physiology, and the presence of co-occurring conditions. Acute withdrawal symptoms, as discussed, typically last days to weeks. However, many individuals experience what is known as Post-Acute Withdrawal Syndrome (PAWS). PAWS symptoms can include mood swings, anxiety, depression, sleep disturbances, fatigue, difficulty concentrating, and cravings, and they can persist for months or even years after acute withdrawal. The brain needs time to slowly re-establish its normal neurotransmitter functions and achieve a new state of balance. Consistent treatment, therapy, a healthy lifestyle, and ongoing support can significantly aid this healing process, though complete “recovery” to a pre-addiction state may be a lifelong journey of management and growth.
Is detox the same as rehab?
No, detox is not the same as rehab, although they are often sequential and complementary parts of the recovery process. Detoxification (or withdrawal management) is the initial, medically supervised process of safely clearing a substance from the body and managing the acute physical and psychological symptoms of withdrawal. It is the first critical step, ensuring safety and stabilizing the individual.
Rehab (rehabilitation), on the other hand, is the comprehensive, longer-term treatment that follows detox. Rehab focuses on addressing the underlying causes of addiction, developing coping mechanisms, and equipping individuals with the tools needed for sustained sobriety. This includes various forms of therapy (individual, group, family), counseling, education on relapse prevention, and skill-building for a sober life. Detox gets the substance out of the body; rehab helps keep it out of the life.
Your First Step Towards a New Life
Overcoming addiction begins with safely navigating Drug Withdrawal. While the process is challenging, it is the gateway to recovery and a healthier future. Professional medical and psychological support is not just helpful—it is often essential for safety and success. You do not have to face this alone. Confidential and anonymous help is available right now. The team at SoberSteps is dedicated to providing resources to guide you through this critical first step. Take control of your life today by calling (844) 491-5566 for a no-obligation, confidential conversation. For more specific information on managing withdrawal from alcohol, explore our detailed guide.



