The Sobering Truth: A Complete Guide to Alcohol Withdrawal
Understand Alcohol Withdrawal: Symptoms, Treatment & Timeline. Learn about safe detox and get help now. Call (844) 491-5566.
Alcohol Use Disorder is a medical condition where a person cannot stop or control their drinking despite serious problems in their life. It’s a brain disorder that affects millions of Americans—not a sign of weakness or lack of willpower.
Quick Facts About Alcohol Use Disorder:
AUD used to be called “alcoholism,” “alcohol abuse,” or “alcohol dependence.” The medical community now uses Alcohol Use Disorder because it better describes the spectrum of the condition and reduces stigma. The disorder causes lasting changes in the brain that make it hard to stop drinking and increase the risk of relapse—but these changes can improve with treatment and time.
Genetics play a significant role, accounting for about 60% of AUD risk. Environmental factors like early drinking, trauma, stress, and mental health conditions like depression or anxiety make up the rest. Starting to drink before age 15 increases the likelihood of developing AUD later in life by more than five times compared to waiting until age 21.
At Sober Steps, we’ve helped thousands of individuals steer their recovery journey from Alcohol Use Disorder by connecting them with evidence-based treatment options and compassionate support. Our mission is to make finding help as private, accessible, and straightforward as possible—because no one should face this alone.
Understanding the signs and symptoms of Alcohol Use Disorder is the first step toward seeking help. AUD is a complex condition that manifests in various ways, impacting an individual’s thoughts, behaviors, and physical health. It’s not always obvious, and sometimes, those closest to the person may be the first to notice changes.
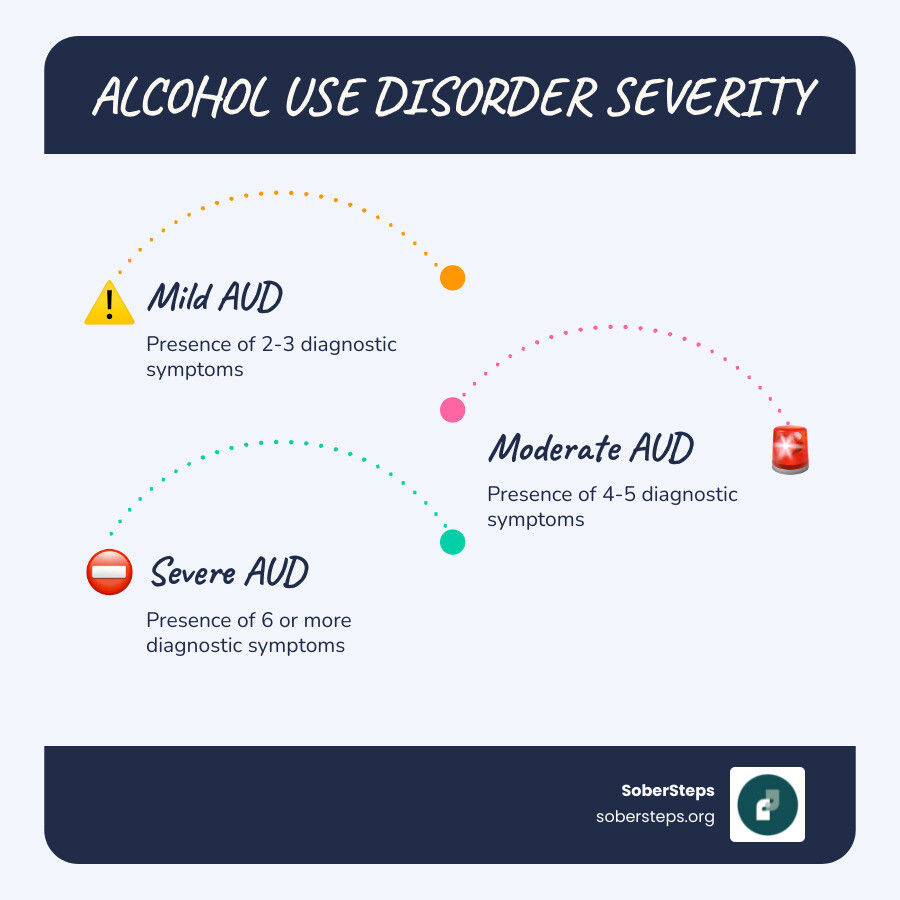
The diagnosis of Alcohol Use Disorder is made by healthcare professionals based on specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). These criteria help us understand the severity of the disorder and guide treatment plans. They broadly fall into categories reflecting impaired control over drinking, social impairment, risky use, and physical effects like tolerance and withdrawal.
Here is a list of the 11 diagnostic criteria for Alcohol Use Disorder, which must be met within a 12-month period:
If you are concerned about your drinking patterns, we encourage you to explore your drinking patterns further. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) provides a helpful resource for self-assessment on their Rethinking Drinking website.
A healthcare professional will assess your symptoms and history to diagnose Alcohol Use Disorder. They will ask you a series of screening questions related to the 11 criteria mentioned above. The number of criteria you meet determines the severity of your AUD:
Even a mild Alcohol Use Disorder can escalate if left unaddressed. Early detection and intervention can make a significant difference in a person’s recovery journey.
Beyond the diagnostic criteria, it’s crucial to understand the immediate effects of alcohol, both during and after consumption, especially heavy or prolonged use.
Signs of Alcohol Intoxication: When someone is intoxicated, alcohol affects their brain and body, leading to:
Alcohol Withdrawal Symptoms: When someone who has been drinking heavily and for a prolonged period suddenly stops or significantly reduces their alcohol intake, they can experience withdrawal. This can be a dangerous, even life-threatening, process and often requires medical supervision. Symptoms can appear within several hours to 4 to 5 days after the last drink and may include:
If you or a loved one are experiencing severe withdrawal symptoms, seek immediate medical attention. Medically supervised detox can help manage these symptoms safely and prevent complications.
Alcohol Use Disorder doesn’t typically have a single cause; rather, it’s often the result of a complex interplay of genetic, psychological, social, and environmental factors. We like to think of it as a puzzle where many pieces come together to form the full picture.
The role of genetics in Alcohol Use Disorder is substantial. Research suggests that hereditability accounts for approximately 60% of the risk for developing AUD. This means that if you have a parent or other close relative who struggles with alcohol, your risk is significantly higher—three to four times higher, in fact. This isn’t about inheriting a “drinking gene” directly, but rather a predisposition. Genes can influence how your body processes alcohol, how you experience its effects, and your vulnerability to its addictive properties.
While genetics lay a foundation, environmental and psychological factors often act as triggers or accelerators for Alcohol Use Disorder.
These factors don’t act in isolation; they often interact in complex ways. For example, someone with a genetic predisposition to AUD who also experiences childhood trauma and later develops depression may face a significantly higher risk.
The impact of Alcohol Use Disorder extends far beyond social and psychological challenges; it can take a severe toll on nearly every organ system in the body. In fact, AUD is the fourth leading preventable cause of death in the U.S. We must understand these health risks to fully grasp the importance of early intervention and treatment.
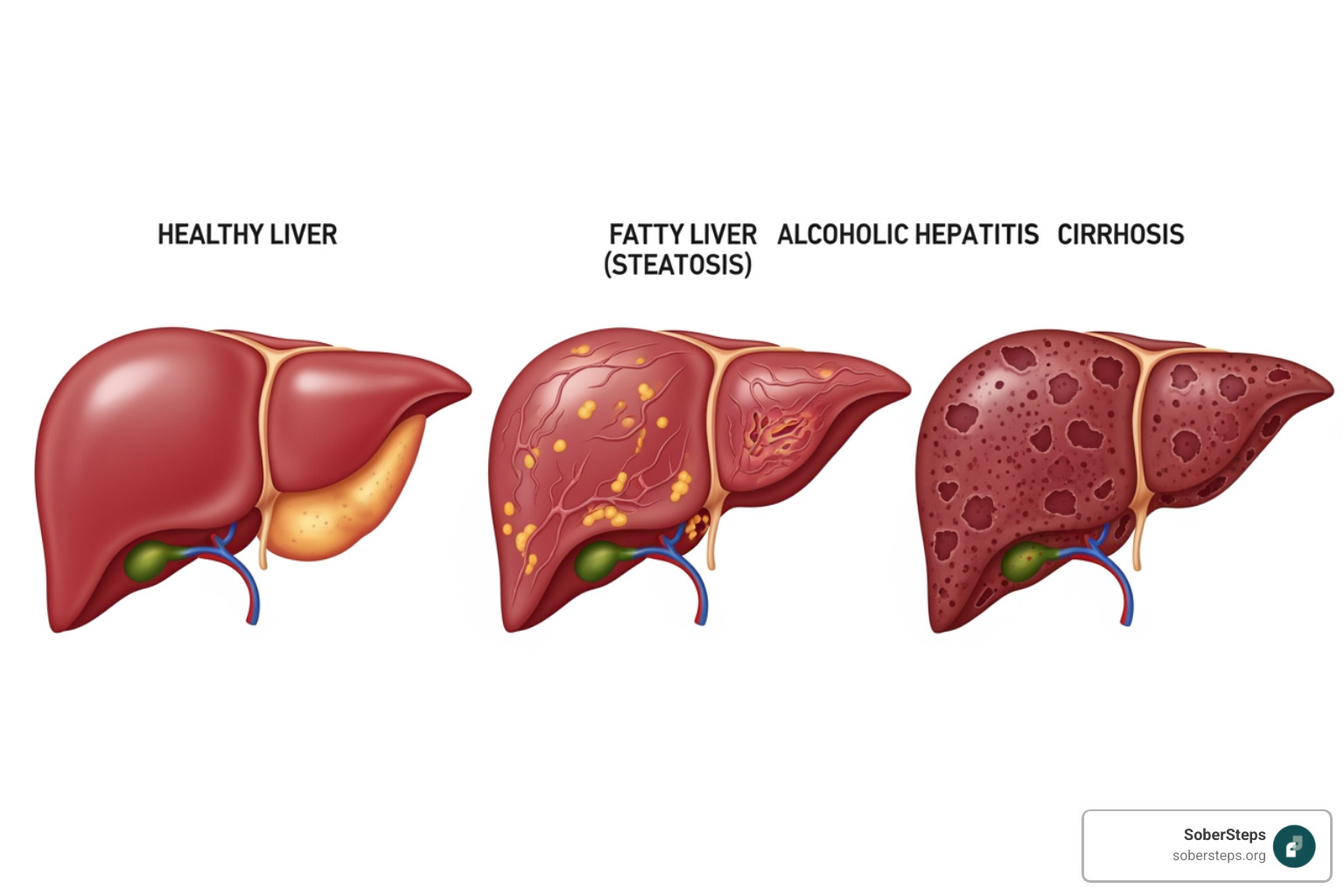
Long-term, excessive alcohol use can lead to a multitude of physical health problems, some of which are irreversible:
The brain is particularly vulnerable to the effects of chronic alcohol exposure:
These health complications underscore the urgency of addressing Alcohol Use Disorder and seeking timely intervention.
The journey to recovery from Alcohol Use Disorder is deeply personal, but one truth shines through: hope is always available, and treatment is effective. We understand that navigating this path can feel overwhelming, but we want you to know that many people with AUD do recover, and their lives transform for the better.
Recovery is not a linear process; setbacks are common and are often part of the journey. What’s crucial is to view these not as failures but as opportunities to learn and adjust your approach. A personalized treatment plan is key, as there’s no one-size-fits-all solution for AUD. We believe in finding the right combination of support, medication, and therapy that works best for each individual.
Medically-Assisted Treatment (MAT) combines medication with counseling and behavioral therapies to provide a comprehensive approach to treating Alcohol Use Disorder. These medications are not addictive themselves and are used under medical supervision to support recovery, reduce cravings, and prevent relapse.
The U.S. Food and Drug Administration (FDA) has approved three medications specifically to help people stop or reduce their drinking:
These medications can be incredibly powerful tools when used as part of a broader treatment plan, helping individuals manage the physical aspects of AUD so they can focus on behavioral and psychological healing.
Behavioral therapies and counseling are cornerstone treatments for Alcohol Use Disorder, helping individuals understand the root causes of their drinking, develop coping skills, and change harmful patterns. These therapies can be delivered individually, in group settings, or even through family sessions.
Some of the most effective behavioral therapies include:
These therapies equip individuals with the tools they need to steer life without relying on alcohol, helping them develop healthier ways to manage stress, emotions, and social situations.
Beyond formal medical and therapeutic interventions, peer support and community resources play a vital role in long-term recovery from Alcohol Use Disorder. These groups offer a sense of belonging, shared experience, and ongoing encouragement.
These groups offer invaluable emotional support, practical advice, and a network of individuals who understand the challenges and triumphs of recovery.
We’ve covered a lot about Alcohol Use Disorder, from its definition as a medical condition and brain disorder to its complex causes, devastating health complications, and diverse treatment options. The most important takeaway is this: Alcohol Use Disorder is a treatable disease, and recovery is not just possible—it’s happening for millions of Americans every day.
Taking the first step can be the hardest, but it’s also the most courageous. Whether you are personally struggling with AUD or are concerned about a loved one, resources are available to help you begin the journey towards a healthier, more fulfilling life.
At SoberSteps, we are dedicated to connecting individuals with the care they need. We understand the importance of privacy and accessibility when seeking help for mental health and substance use disorders. Our platform is designed to be a confidential, anonymous online resource that guides you to appropriate treatment options.
If you are ready to take that crucial first step, or if you are looking for support for someone you care about, please reach out. We can help you find the right path forward.
You don’t have to face this alone. Help is available, and a life in recovery is within reach.
Understand Alcohol Withdrawal: Symptoms, Treatment & Timeline. Learn about safe detox and get help now. Call (844) 491-5566.
Discover powerful addiction success stories of triumph & new beginnings. Find hope & take your first step to recovery.

Your guide to confidential mental health support. Learn privacy rights, recognize signs, and find trusted, private care. Call (844) 491-5566.
For anyone seeking help for addiction for themselves or a loved one calls to Sober Steps are completely confidential and available 24/7.
Please note: any treatment center listed on our site that receives calls is a paid advertiser.
Calls to a specific treatment center’s listing will be connected directly to that center.
Calls to our general helpline will be answered by treatment providers, all of whom are paid advertisers.
By calling the helpline, you agree to our terms and conditions. These calls are free of charge and carry no obligation to enter treatment. Neither Sober Steps nor anyone answering your call receives a commission or fee based on your choice of treatment provider.
If you’d like to explore additional treatment options or connect with a specific rehab center, you can browse our top-rated listings, visit our homepage, or call us at (844) 491-5566. You may also contact us for further assistance.