
When Medication Becomes a Trap: Understanding Benzodiazepine Withdrawal Anxiety
Benzodiazepine withdrawal anxiety is one of the most challenging and often unexpected symptoms people face when stopping or reducing medications like Xanax, Klonopin, or Valium. If you’re searching for information on this topic, here’s what you need to know right now:
Key Symptoms of Benzodiazepine Withdrawal Anxiety:
- Intense anxiety and panic attacks that may be worse than your original symptoms
- Physical symptoms including insomnia, muscle tension, tremors, sweating, and heart palpitations
- Psychological symptoms like irritability, poor concentration, restlessness, and depression
- Sensory disturbances such as increased sensitivity to light and sound
- Timeline varies: Symptoms typically start within 24 hours to 3 weeks after stopping, depending on the medication’s half-life
Critical Facts:
- Approximately 40% of long-term users experience moderate to severe withdrawal symptoms
- About 10% may experience protracted withdrawal lasting months or even years
- Withdrawal can be dangerous – seizures and severe symptoms require medical supervision
- Gradual tapering under medical guidance is the safest approach
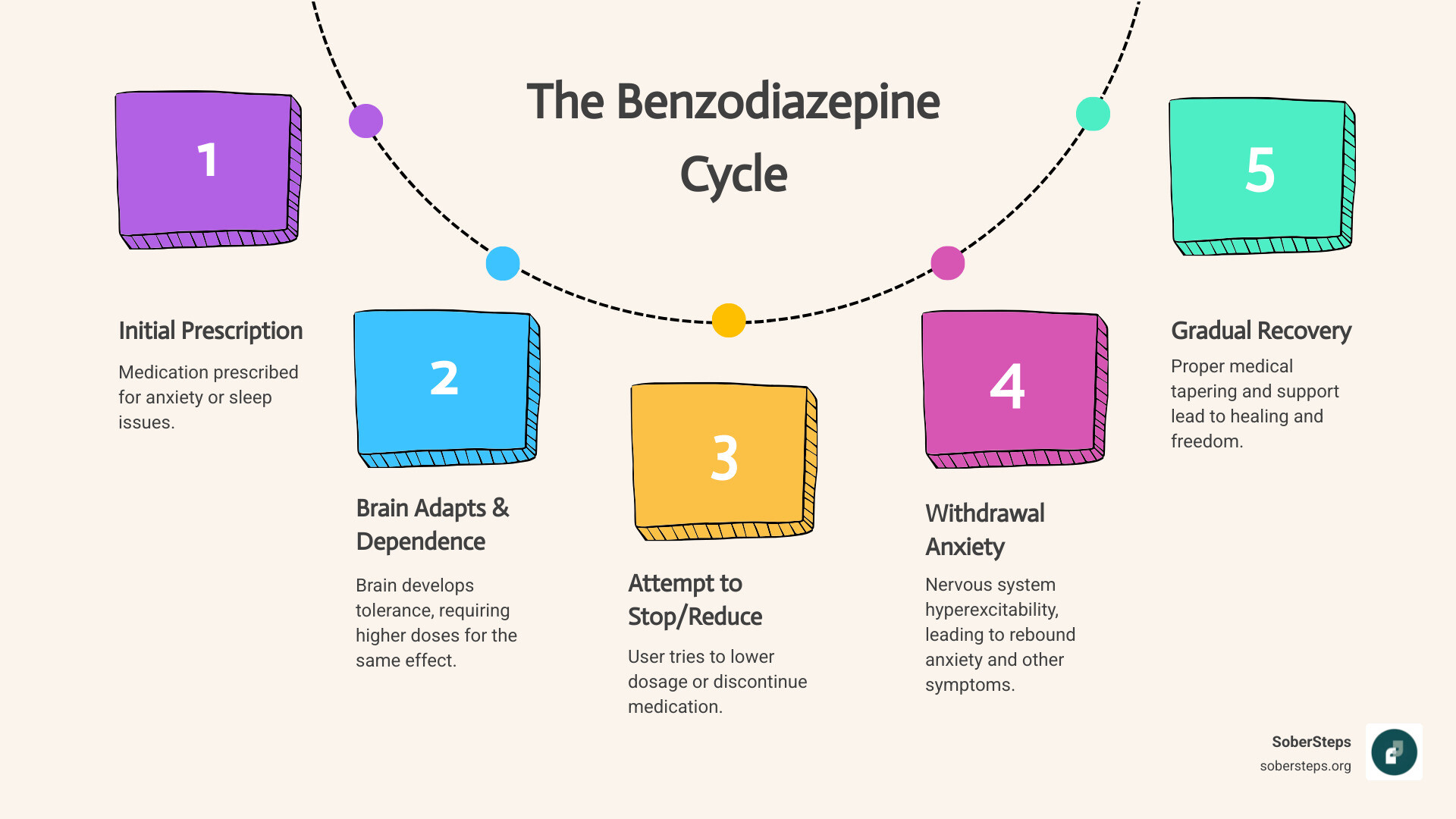
Benzodiazepines were prescribed to help with anxiety or sleep problems, but your brain adapted to their presence over time. When you reduce or stop taking them, your nervous system becomes temporarily hyperactive, creating a surge of anxiety that can feel overwhelming. This isn’t a sign of weakness or failure – it’s a predictable physiological response to physical dependence.
The good news? Recovery is possible. With proper medical support, a carefully managed tapering schedule, and the right coping strategies, you can steer this challenging period and regain control of your life without benzodiazepines.
At Sober Steps, we’ve supported countless individuals through the complexities of benzodiazepine withdrawal anxiety, providing evidence-based information to help you understand what’s happening and find the right path forward. Whether you’re just beginning to consider tapering or you’re already experiencing withdrawal symptoms, our confidential helpline can connect you with resources custom to your situation.
In this guide, we’ll walk you through everything you need to know about benzodiazepine withdrawal anxiety – from understanding why it happens to practical strategies for managing symptoms safely.
Understanding Benzodiazepine Withdrawal Anxiety: Symptoms and Timeline
When we talk about benzodiazepine withdrawal anxiety, we’re referring to a complex set of reactions your body and mind can experience when you reduce or stop taking benzodiazepine medications. These medications, often called “benzos,” are powerful central nervous system depressants prescribed for conditions like anxiety, insomnia, seizures, and muscle spasms. While effective in the short term, prolonged use can lead to physical dependence, making withdrawal a challenging journey.
The experience of benzodiazepine withdrawal anxiety can be intense and varied, often encompassing both psychological and physical symptoms that can profoundly impact daily life. Understanding these symptoms and their typical timeline is the first step toward effective management and recovery. If you’re struggling with these symptoms, support is available for withdrawal symptoms.
Key Psychological and Physical Symptoms
The withdrawal syndrome associated with benzodiazepines is characterized by a wide array of symptoms. Many of these mirror the very conditions the medication was initially prescribed to treat, but often with heightened intensity. This can be especially disorienting and frightening.
Here are the primary psychological and physical symptoms we often see with benzodiazepine withdrawal anxiety:
Psychological Symptoms:
- Intense anxiety: This is often the most prominent symptom, manifesting as overwhelming feelings of dread, worry, and apprehension. It can feel far worse than any pre-existing anxiety.
- Panic attacks: Sudden, severe episodes of intense fear accompanied by physical symptoms like a racing heart, shortness of breath, and dizziness.
- Irritability: A heightened sense of frustration and anger, leading to emotional outbursts.
- Depression: Feelings of sadness, hopelessness, and a loss of interest in activities once enjoyed. Some evidence suggests that higher benzodiazepine dosages can even increase depression, and reducing or discontinuing therapy may resolve these symptoms.
- Poor concentration: Difficulty focusing, remembering information, and maintaining attention.
- Memory problems: Issues with both short-term recall and forming new memories. Long-term users often experience cognitive impairment and memory issues, which can persist even after withdrawal.
- Restlessness: An inability to sit still, feeling constantly on edge or agitated.
- Agoraphobia: A fear of situations that might cause panic, helplessness, or embarrassment, often leading to avoidance of open or crowded spaces.
- Depersonalization/Derealization: Feelings of detachment from one’s body, thoughts, or surroundings, making reality feel unreal or dreamlike.
Physical Symptoms:
- Insomnia: Significant difficulty falling or staying asleep, often leading to severe sleep deprivation. Chronic benzodiazepine use disrupts sleep architecture and diminishes deep sleep time.
- Muscle pain and stiffness: Aches, spasms, and tension throughout the body.
- Headaches: Ranging from mild tension headaches to severe migraines.
- Sweating: Excessive perspiration, sometimes accompanied by hot or cold flashes.
- Heart palpitations: A sensation of a racing, pounding, or irregular heartbeat.
- Nausea (feeling sick) and Vomiting (being sick): Gastrointestinal distress, sometimes accompanied by abdominal cramps, diarrhea, or constipation.
- Tremors: Involuntary shaking, particularly in the hands.
- Increased sensitivity: Heightened reactions to light, noise, touch, and smell.
- Tinnitus: Ringing, buzzing, or other noises in the ears.
- Seizures (severe cases): One of the most dangerous potential symptoms, especially with abrupt cessation. Generalized tonic-clonic seizures (grand mal seizures) can occur and are potentially fatal.
These symptoms can vary in intensity and combination, making each person’s withdrawal experience unique. The National Institute on Drug Addiction describes the withdrawal syndrome as “typically characterized by sleep disturbance, irritability, increased tension and anxiety, panic attacks, hand tremor, sweating, difficulty in concentration, dry wretching and nausea, some weight loss, palpitations, headache, muscular pain and stiffness and a host of perceptual changes.” More serious developments like seizures and psychotic reactions are reported in high-dosage withdrawals.
How Withdrawal Anxiety Differs from a Pre-Existing Anxiety Disorder
It’s common for individuals to wonder if the anxiety they experience during withdrawal is simply their original anxiety disorder returning. However, benzodiazepine withdrawal anxiety is distinct and often more severe than a pre-existing anxiety disorder. This distinction is crucial for proper diagnosis and management.
One key difference is “rebound anxiety.” This is an increase in anxiety upon stopping benzodiazepines, often worse than the original symptoms they were prescribed to treat. It’s a direct physiological response to the brain’s adjustment after the drug is removed. This rebound effect can be intense and disorienting, making it feel like your anxiety has come back with a vengeance. We’ve seen that if they’re used incorrectly, rebound anxiety can be particularly severe.
Beyond intensification, withdrawal can introduce entirely new symptoms that weren’t part of your original anxiety profile. These might include sensory disturbances, depersonalization, or severe physical discomforts like muscle pain and tinnitus. These new symptoms are hallmarks of the withdrawal syndrome itself, not just a return of the underlying condition.
Distinguishing between withdrawal and a relapse of a pre-existing anxiety disorder is vital. A misdiagnosis can lead to continuing benzodiazepine use, prolonging dependence, or inappropriate treatment. Healthcare professionals need to recognize the unique characteristics of withdrawal to avoid these pitfalls. For a deeper dive into the complexities, you can explore scientific research on the benzodiazepine withdrawal syndrome.
Pre-existing anxiety disorders can indeed influence the experience of benzodiazepine withdrawal anxiety, often making it more challenging. Individuals with a history of severe anxiety or panic attacks may perceive withdrawal symptoms as particularly threatening, amplifying their distress. This highlights the importance of comprehensive support that addresses both the physiological and psychological aspects of withdrawal. If you have co-occurring mental health challenges, getting help for co-occurring disorders is essential for a holistic recovery.
The Withdrawal Timeline: From Acute to Protracted Symptoms
The timeline for benzodiazepine withdrawal anxiety is highly variable, influenced by factors like the specific benzodiazepine used, its dosage, and the duration of use. However, we can generally outline three phases: early, acute, and protracted withdrawal.
For short-acting benzos like Xanax, withdrawal symptoms can begin quite quickly, often within 6-24 hours after the last dose. This rapid onset is due to the drug leaving the system quickly. Symptoms typically peak around 2-5 days and can last for about 2 weeks.
For long-acting benzos like Valium, the onset of withdrawal is slower, usually starting between 2-10 days after the last dose, but can sometimes be delayed up to three weeks. This is because these medications stay in your system longer. Symptoms typically peak around 2-3 weeks and can last for several weeks to months. Most benzodiazepine withdrawal symptoms start within 24 hours and can last from a few days to several months, depending on the strength of the benzo used.
The acute phase of withdrawal generally refers to the period of most intense symptoms, which can last from several weeks to a few months. During this time, the body is actively trying to re-establish its natural balance without the drug.
However, for some individuals, symptoms can persist much longer. This is known as Protracted Withdrawal Syndrome (PAWS). We know that some people, around 10 percent according to a study, may experience PAWS that can extend several months or even years after stopping use of a benzodiazepine. About 10 percent of people who abuse benzos still feel withdrawal symptoms years after they have stopped taking the drugs.
PAWS is characterized by fluctuating symptoms, often described as “waves and windows.” During a “wave,” symptoms like intense anxiety, insomnia, cognitive deficits, depression, and mood swings can return with force. A “window” is a period of relative calm where symptoms subside, offering a glimpse of recovery. This unpredictable nature of PAWS can be incredibly frustrating and demoralizing, making consistent support and patience essential. For more detailed insights, you can review expert analysis of protracted withdrawal syndromes90023-4).
The Science Behind the Anxiety: Why Withdrawal Happens
Understanding “why” your body reacts the way it does during benzodiazepine withdrawal anxiety can help explain the experience and reinforce the importance of a structured approach to recovery. It’s not just “in your head”; there are profound neurobiological changes at play.
Benzodiazepines exert their calming effects by interacting with specific neurotransmitter systems in your brain. When these medications are removed, your brain, which has adapted to their presence, struggles to regain its natural equilibrium, leading to a state of hyperexcitability. To learn more about how addiction affects the brain, visit our page on the science of addiction.
How Benzodiazepines Change Your Brain’s Chemistry
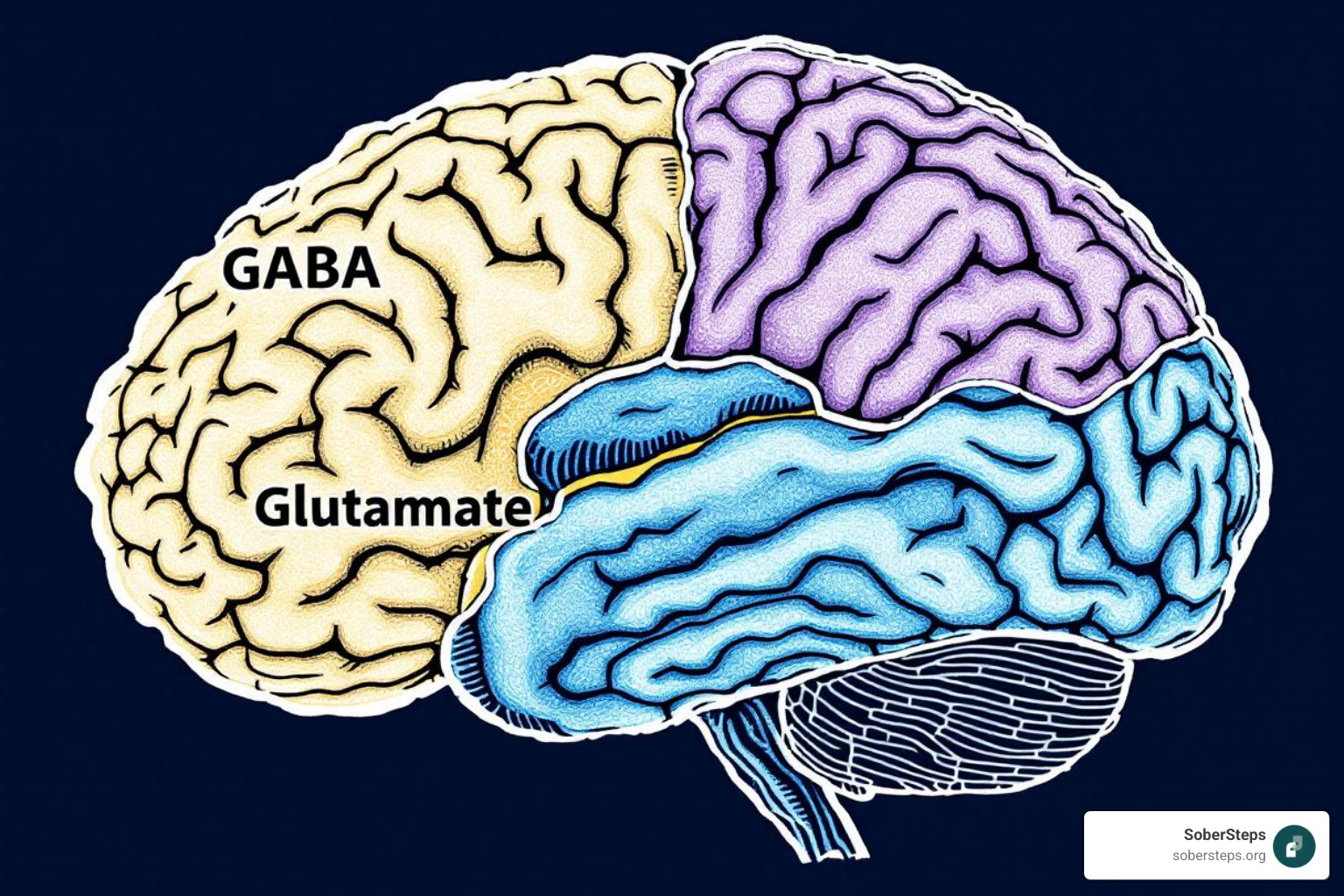
At the heart of benzodiazepine withdrawal anxiety is the brain’s GABA (gamma-aminobutyric acid) system. GABA is the primary inhibitory neurotransmitter in the central nervous system. Its role is to slow down brain activity, promoting relaxation, reducing anxiety, and aiding sleep. Benzodiazepines work by enhancing the effect of GABA, essentially putting a brake on overactive brain signals. They do this by increasing the frequency of chloride channel opening on GABA-A receptors, allowing more chloride ions to enter neurons, which makes them less likely to fire. This is why benzos are so effective at calming panic attacks and promoting sleep.
However, with prolonged use, your brain begins to adapt to this constant “brake.” This leads to tolerance development, where your brain becomes less sensitive to GABA’s inhibitory effects, requiring higher doses of the benzodiazepine to achieve the same calming outcome. This adaptation also involves a process called GABA receptor downregulation, where the number or sensitivity of GABA receptors decreases.
When benzodiazepines are then reduced or stopped, this adapted system is suddenly left without its usual external boost. The GABA system is now less effective at dampening brain activity, and the brain’s excitatory systems, primarily mediated by glutamate (the most abundant excitatory neurotransmitter), rebound. This leads to an excitatory surge, a state of central nervous system hyperexcitability that manifests as the intense anxiety, restlessness, insomnia, and even seizures characteristic of benzodiazepine withdrawal anxiety. Neuroadaptive processes involving both GABAergic and glutamatergic systems are deeply implicated in tolerance, dependence, and withdrawal. The brain is literally struggling for balance.
Risk Factors That Influence Withdrawal Severity
Not everyone experiences benzodiazepine withdrawal anxiety with the same intensity or duration. Several factors can significantly influence the severity and persistence of withdrawal symptoms:
- Type of Benzodiazepine:
- Potency: Higher potency benzodiazepines (e.g., Xanax) can lead to more severe withdrawal symptoms.
- Half-life: Short-acting benzodiazepines (e.g., Xanax) leave the body quickly, leading to an earlier and often more intense onset of withdrawal symptoms. Long-acting benzodiazepines (e.g., Valium) have a slower, more gradual withdrawal, which can sometimes be less acute but more prolonged. Short-acting benzos can be particularly difficult to come off if taken for a long time.
- Duration of Use: The longer you take benzodiazepines, the more likely you are to develop physical dependence and experience withdrawal symptoms. Dependency rates are much higher, at 20% to 45%, after more than a year of use. Few users become dependent with less than three months of use.
- Dosage Level: Higher doses typically lead to more severe withdrawal. For instance, patients taking 4 mg/day or higher of Xanax for longer than three months were more likely to become dependent and experience more uncomfortable withdrawal symptoms.
- Abrupt Cessation vs. Tapering: Quitting “cold turkey” or stopping abruptly is a major risk factor for severe, potentially dangerous withdrawal symptoms, including seizures. Gradual tapering is crucial for mitigating severity.
- Pre-existing Anxiety Disorders: As we discussed, a history of anxiety can make the experience of withdrawal anxiety more challenging and distressing.
- Individual Physiology: Each person’s unique metabolism, genetics, and overall health status can influence how they respond to withdrawal.
- Concurrent Substance Use: Dependence on alcohol or other sedatives can increase the risk of benzodiazepine dependence and complicate withdrawal.
Understanding these risk factors allows us to better anticipate and prepare for the challenges of benzodiazepine withdrawal anxiety, emphasizing the need for individualized, medically supervised approaches.
A Practical Guide to Managing Withdrawal Anxiety
Navigating benzodiazepine withdrawal anxiety can feel like climbing a mountain, but you don’t have to do it alone. With the right strategies and support, we can help you find your way to a calmer, benzo-free future. The cornerstone of safe and effective withdrawal is medical supervision, coupled with robust coping mechanisms.
If you’re ready to take the first step, finding a detox program that can help you taper safely is one of the best decisions you can make.
The Gold Standard: Medically-Supervised Gradual Tapering
When it comes to managing benzodiazepine withdrawal anxiety, medically-supervised gradual tapering is considered the “gold standard.” This approach prioritizes safety and minimizes the intensity of withdrawal symptoms by slowly reducing the medication dose over time.
- Why Tapering is Essential: Abruptly stopping benzodiazepines, or going “cold turkey,” is not only incredibly uncomfortable but can be dangerous and even life-threatening due to the risk of severe seizures. Tapering allows your brain to gradually readjust to the absence of the drug, reducing the excitatory surge we discussed earlier. The British National Formulary recommends withdrawing too slowly rather than too quickly from benzodiazepines.
- The Ashton Manual: This widely recognized protocol, developed by Professor Heather Ashton, advocates for a very slow, individualized taper, often involving switching from a short-acting benzodiazepine to a longer-acting one, such as diazepam. Diazepam is often preferred because its long half-life provides a smoother, more stable reduction in drug levels, minimizing sharp fluctuations that can trigger severe withdrawal.
- Individualized Tapering Schedules: There is no one-size-fits-all approach. The rate of taper depends on the severity of withdrawal symptoms, which are influenced by several factors: the type of benzo, dosage, duration of use, and individual response. Medical providers will adjust the tapering speed to your tolerance to minimize discomfort. The American Society of Addiction Medicine (ASAM) recommends an initial taper pace of 5-10% reduction every 2-4 weeks, emphasizing that a taper that is too rapid can be dangerous and potentially life-threatening.
- Slow and Steady Dose Reduction: This might mean reducing your dose by a small percentage every few weeks or even months. The goal is to make each step manageable, ensuring that your body has time to adapt before the next reduction. We often say, “Withdraw too slowly rather than too quickly.”
Medical supervision is crucial throughout this process. Your healthcare provider can monitor your symptoms, adjust the taper schedule as needed, and provide support to ensure your safety and comfort.
Pharmacological Support for benzodiazepine withdrawal anxiety
While tapering is the main event, several adjunctive medications can provide valuable support in managing specific symptoms of benzodiazepine withdrawal anxiety. These are not meant to replace the taper itself but to make the journey more tolerable.
- Anticonvulsants: Medications like carbamazepine or gabapentin may be prescribed to help stabilize brain activity and reduce the risk of seizures, particularly during the initial phases of withdrawal.
- Beta-blockers: Drugs like propranolol can help manage physical symptoms of anxiety, such as a racing heart, tremors, and sweating, without affecting the underlying anxiety directly.
- Non-addictive Anxiety Medications: Buspirone, a non-benzodiazepine anxiolytic, might be introduced to help manage anxiety symptoms as the benzodiazepine dose decreases. Antidepressants, particularly SSRIs, might also be considered for co-occurring depression or anxiety, though some research suggests they may not be effective for depression directly caused by benzodiazepine withdrawal.
- Importance of Medical Consultation: It’s absolutely critical that any pharmacological support is managed by a healthcare professional. Combining medications, or using them inappropriately, can lead to adverse effects or complicate the withdrawal process. For instance, antipsychotics are generally avoided during withdrawal as they can aggravate symptoms, including convulsions. Similarly, certain antibiotics like fluoroquinolones should be contraindicated in patients dependent on or in benzodiazepine withdrawal, as they can increase CNS toxicity.
There are significant challenges in pharmacological management of benzodiazepine withdrawal, making expert guidance indispensable. If you’re considering these options, please talk to a professional about your options.
Non-Pharmacological Strategies for Coping with benzodiazepine withdrawal anxiety
While medical and pharmacological interventions address the physiological aspects, non-pharmacological strategies are indispensable for managing the psychological distress and enhancing overall well-being during benzodiazepine withdrawal anxiety. These tools empower you to actively participate in your healing process.
- Cognitive-Behavioral Therapy (CBT): CBT is an evidence-based therapy that helps you identify and change negative thought patterns and behaviors that contribute to anxiety. It equips you with coping skills to manage symptoms, reduce fear, and prevent relapse. A Cochrane review found CBT plus taper was effective in achieving discontinuation in the short-term.
- Peer Support Groups: Connecting with others who understand your experience can be incredibly validating and empowering. Groups like Narcotics Anonymous (NA) offer a sense of community and shared experience, providing encouragement and practical advice.
- Stress Management Techniques: Learning to manage stress is vital. This can include:
- Meditation and Mindfulness: Practices that help you stay present and observe anxious thoughts without judgment, reducing their power.
- Deep Breathing Exercises: Simple techniques that can calm your nervous system and reduce acute anxiety.
- Yoga and Tai Chi: Gentle forms of exercise that combine physical movement with breathwork and mindfulness, promoting relaxation.
- Regular Exercise: Physical activity can be a powerful antidote to anxiety and depression, releasing endorphins and improving mood. Even a brisk walk can make a difference.
- Balanced Nutrition: A healthy diet supports overall brain function and can help stabilize mood and energy levels. Avoiding excessive caffeine (which can worsen withdrawal symptoms) and sugar is often recommended.
- Sleep Hygiene: Establishing a consistent sleep routine, creating a comfortable sleep environment, and avoiding screens before bed can improve sleep quality, which is often severely disrupted during withdrawal.
These strategies, when integrated into a comprehensive treatment plan, can significantly reduce the burden of benzodiazepine withdrawal anxiety and help build resilience for long-term recovery. For those interested in exploring these approaches further, we offer resources on holistic therapy options.
Frequently Asked Questions about Benzodiazepine Withdrawal Anxiety
We understand you likely have many questions about benzodiazepine withdrawal anxiety. Here are some of the most common ones we encounter:
How long does the intense anxiety from benzo withdrawal last?
The most intense, or “acute,” phase of anxiety can last from several weeks to a few months. During this period, your body is undergoing significant readjustment, and symptoms can be quite severe. However, for a smaller percentage of individuals, symptoms like anxiety can persist in waves for many months or even years. This is known as Protracted Withdrawal Syndrome (PAWS). Approximately 10% of people who stop benzodiazepines may experience PAWS, where symptoms fluctuate but gradually improve over time. While challenging, these symptoms are temporary and will eventually subside.
Can I just switch to a different anxiety medication?
This should only be done under strict medical supervision. While some non-addictive medications may help manage symptoms, they are not a substitute for a proper benzodiazepine taper. Abruptly stopping a benzodiazepine, even while starting another medication, can still trigger severe withdrawal symptoms, including seizures. Your healthcare provider might consider switching you to a longer-acting benzodiazepine (like diazepam) as part of a tapering plan, but this is a carefully managed process, not a simple swap. Always consult with your doctor before making any changes to your medication regimen.
Will I ever feel “normal” again?
Yes! While the withdrawal process is undoubtedly difficult and can be lengthy, the brain has a remarkable capacity to heal, a phenomenon known as neuroplasticity. With a proper, medically supervised taper, strong support, and healthy coping strategies, it is absolutely possible to recover fully and manage anxiety without benzodiazepines. Studies have shown significant improvements in cognitive function and overall well-being after successful withdrawal. For instance, one study found that after one year of abstinence from long-term use of benzodiazepines, cognitive, neurological, and intellectual impairments had returned to normal. Recovery is a journey, but a benzo-free future where you feel like yourself again is achievable. Learn about long-term recovery support to help maintain your progress.
Conclusion: Your Path to a Calmer, Benzo-Free Future
Navigating benzodiazepine withdrawal anxiety is one of the most challenging experiences someone can face, but it is also a profound journey toward reclaiming your health and well-being. We’ve explored the intricate dance between your brain chemistry and these powerful medications, understanding why withdrawal happens, what symptoms to expect, and how to approach recovery safely and effectively.
Withdrawal is a process, not a single event. The timeline varies, symptoms can be intense, and the path may have its ups and downs, especially with the possibility of protracted withdrawal. However, the consistent message from medical experts and those who have successfully steerd this journey is clear: medical supervision is critical. A gradual, individualized tapering plan, combined with pharmacological support and non-pharmacological coping strategies like CBT and peer support, offers the safest and most effective route to recovery.
The brain’s remarkable capacity to heal and adapt means that a calmer, benzo-free future is not just a dream—it’s an achievable reality. At SoberSteps, we are an independent resource dedicated to helping you understand your options and connect with the support you need. Your well-being is our priority, and we believe in your strength to overcome this challenge.
If you or a loved one are struggling with benzodiazepine withdrawal anxiety or considering tapering off benzodiazepines, please don’t hesitate. Call our 24/7 confidential helpline to explore your recovery options today. We are here to guide you every step of the way.


