Understanding the Overlap: What Are Co-Occurring Disorders?
Mental health and substance use co occurring disorders occur when a person experiences both a mental health condition and a substance use disorder at the same time. This is also known as dual diagnosis.
Quick Facts About Co-Occurring Disorders:
- Definition: Having at least one mental health disorder (like depression, anxiety, or PTSD) alongside at least one substance use disorder (alcohol, drugs, or prescription medication misuse)
- How Common: More than one in four adults with serious mental health problems also has a substance use problem
- The Connection: These conditions often influence each other—mental health issues can lead to substance use as a form of self-medication, while substance use can trigger or worsen mental health symptoms
- Why It Matters: Treating only one condition usually doesn’t work; both need to be addressed together for successful recovery
If you or someone you love is struggling with both mental health challenges and substance use, you’re not alone. In fact, research shows that as many as 65% of people with alcohol and drug addictions also suffer from co-occurring mental health disorders. The relationship between these conditions is complex—they share common risk factors like genetics, trauma, and brain chemistry changes, and they often create a cycle where each condition makes the other worse.
Recognizing co-occurring disorders is the first critical step toward recovery. Many people don’t realize they’re dealing with both conditions, or they may receive treatment for only one issue while the other goes unaddressed. This guide will help you understand how these conditions connect, recognize the warning signs, and explore the integrated treatment approaches that offer the best hope for lasting recovery.
At Sober Steps, we’ve helped thousands of individuals and families steer the complexities of mental health and substance use co occurring disorders through our comprehensive resources, treatment directories, and supportive community. Our mission is to provide you with reliable, confidential information that empowers you to take the next step toward healing.
The Complex Connection: Why Mental Health and Substance Use Disorders Occur Together
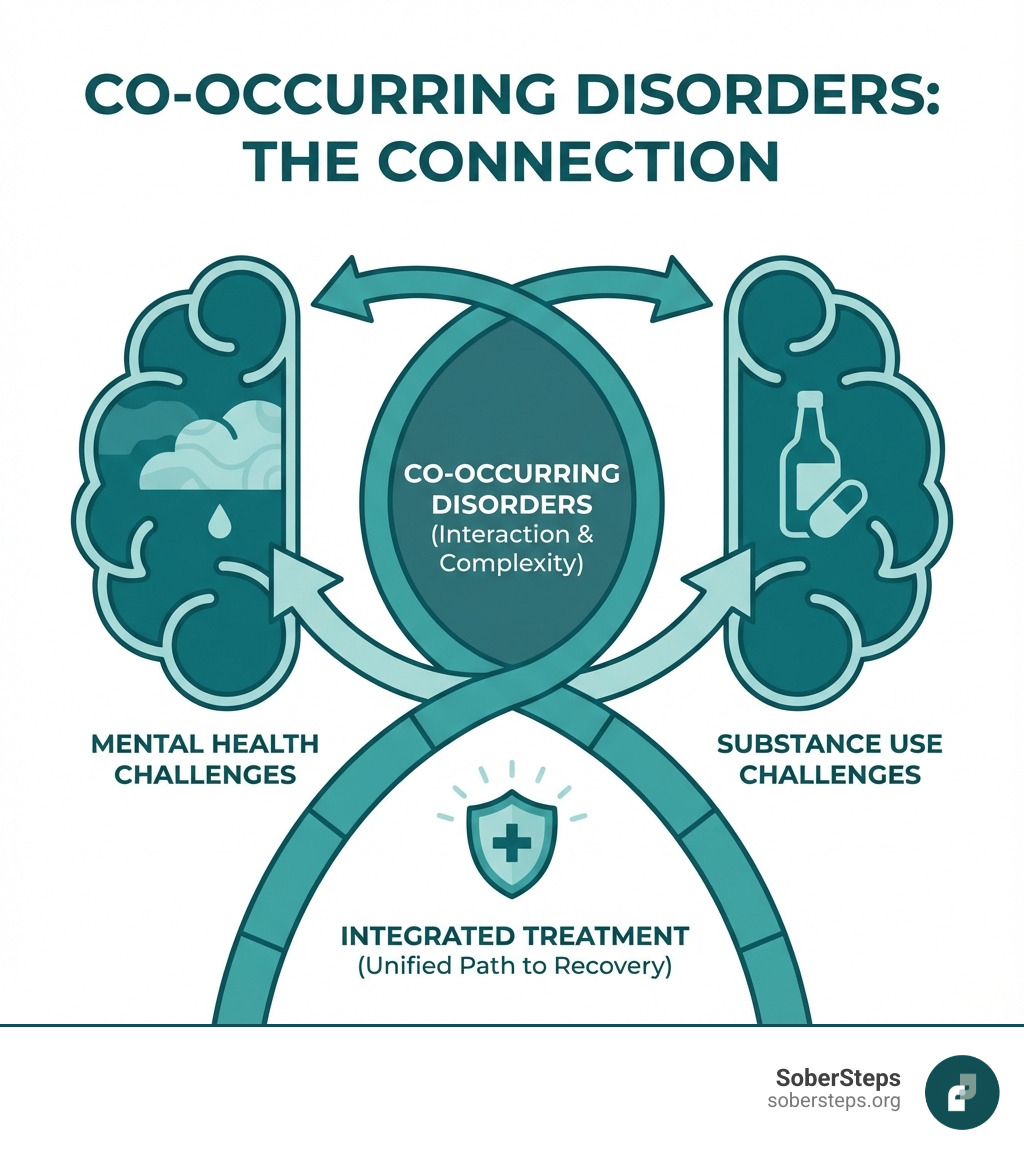
It’s a common misconception that one condition directly “causes” the other. In reality, the relationship between mental health and substance use co occurring disorders is a complex, bidirectional street. They often share common origins and can significantly influence each other’s development and severity.
Why do these two worlds collide so frequently? We can point to several interconnected factors:
- Shared Risk Factors: Just like siblings might share a family resemblance, these disorders often share common risk factors. These include inherited genetic predispositions, adverse social environments, and chronic stress or trauma. For example, over 30% of adults with a substance use disorder (SUD) have experienced childhood trauma.
- Genetics: Our genes can play a significant role. Research suggests there are genetic risk factors that can make an individual more vulnerable to both certain mental health disorders and substance use disorders.
- Environmental Factors: Our surroundings and life experiences contribute heavily. Exposure to stress, poverty, social isolation, or loss can act as triggers. A stressful environment can also activate genetic predispositions, making someone more susceptible to developing these conditions.
- Self-Medication Hypothesis: This is a powerful theory. Many individuals with undiagnosed or untreated mental health issues turn to substances as a way to cope with their symptoms. Feeling anxious? A drink might temporarily quiet the nerves. Struggling with depression? Opioids might offer a fleeting sense of euphoria. While substances might offer temporary relief, they ultimately worsen the underlying mental health problems in the long run.
- Substance-Induced Mental Disorders: Substances themselves can directly cause or worsen mental health symptoms. For instance, heavy alcohol use can lead to depression, while stimulant abuse can trigger paranoia or psychosis. These are not independent mental health conditions but rather direct consequences of substance use.
- Brain Chemistry Changes: Both mental health disorders and substance use disorders involve changes in brain structure and function. They can impact similar neural circuits related to reward, stress, and self-control. For example, dysregulation in frontal-limbic systems, which manage emotions and impulses, is linked to both depression and substance use disorders. This shared neurobiology can create a vicious cycle, where one condition makes the brain more vulnerable to the other. You can dig deeper into The neurobiology of co-occurring disorders for more information.
Understanding this intricate connection is vital for effective treatment. It underscores why an integrated approach, addressing both conditions simultaneously, is not just helpful but essential for lasting recovery. Learn more about the intricacies of Dual Diagnosis.
Common Co-Occurring Pairings
While any mental health condition can co-occur with any substance use disorder, some pairings are particularly common and well-studied. These are not exhaustive lists, but they highlight the significant overlap:
- Depression and Alcoholism: This is one of the most frequently observed pairings. Up to 80% of individuals with alcohol use disorder experience depressive symptoms at some point, and 30% meet the criteria for major depression. People may drink to numb feelings of sadness or hopelessness, which then exacerbates depressive episodes. For more specific insights, visit Dual Diagnosis Depression.
- Anxiety and Benzodiazepine Use: Anxiety disorders (like generalized anxiety, panic disorder, or social anxiety) are prevalent among those with SUDs, with rates ranging from 10% to 60% in treatment populations. Individuals often use benzodiazepines (like Xanax or Klonopin) or alcohol to alleviate anxiety, leading to dependence and worsening anxiety over time. Find more about Dual Diagnosis Anxiety.
- PTSD and Opioid Use: Post-Traumatic Stress Disorder (PTSD) is strongly linked to substance use. As many as one-third of patients entering SUD treatment meet criteria for PTSD. Estimates of lifetime prevalence of SUDs in civilian populations with PTSD range from 22% to 43%. People with PTSD may use opioids or other substances to self-medicate the intense emotional pain, flashbacks, and hyperarousal associated with trauma. Explore Dual Diagnosis PTSD.
- Bipolar Disorder and Cocaine Use: Individuals with bipolar disorder often struggle with substance use, with cocaine being particularly common during manic episodes due to its stimulating effects. However, cocaine use can worsen bipolar symptoms, triggering more severe mood swings and rapid cycling. Gain a deeper understanding at Dual Diagnosis Bipolar Disorder.
- Schizophrenia and Nicotine Dependence: Up to 50% of individuals with schizophrenia have either alcohol or illicit drug dependence, and more than 70% are nicotine dependent. Nicotine is often used to cope with the negative symptoms of schizophrenia or as a form of self-medication for medication side effects.
Recognizing the Signs and Navigating Diagnosis
Identifying mental health and substance use co occurring disorders can be tricky, both for individuals and for healthcare professionals. The symptoms often overlap, mask each other, or can be attributed solely to one condition, leading to misdiagnosis or delayed treatment.
Why is Diagnosing Co-Occurring Disorders Challenging?
- Symptom Overlap: Many symptoms of mental health disorders, like mood swings, sleep disturbances, or paranoia, can also be caused by substance use or withdrawal. This makes it difficult to discern the primary issue. For instance, is someone depressed because of their alcohol use, or are they drinking heavily because they’re depressed?
- Masking Effects: One condition can mask the severity of the other. A person might focus on treating their substance use, believing that once they stop, their mental health will magically improve, only to find that underlying issues persist. Conversely, mental health symptoms can be so overwhelming that substance use is overlooked or downplayed.
- Denial: Denial is a powerful force in both addiction and mental illness. Individuals might minimize their substance use or dismiss their mental health struggles, making it harder for them to seek help or for others to identify the problem.
- Complexity: Psychiatric diagnosis is inherently complex, and there are no simple lab tests for most mental health conditions. When substance use is involved, it adds another layer of complexity, requiring experienced professionals to conduct comprehensive assessments.
Given these challenges, the importance of a professional, comprehensive assessment cannot be overstated. A healthcare provider experienced in both mental health and substance use disorders is best equipped to make an accurate diagnosis. If you’re seeking help, consider exploring Confidential Mental Health Support.
Signs of a Substance Use Disorder
Recognizing the signs of a substance use disorder is a crucial first step. These signs can manifest in behavioral, physical, and social ways:
- Behavioral Signs:
- A noticeable drop in performance or attendance at work or school.
- Frequent trouble-making or engaging in secretive behaviors.
- Significant changes in appetite or sleep patterns.
- Dramatic personality shifts or sudden, intense mood swings.
- A pervasive lack of motivation or enthusiasm.
- Appearing fearful, anxious, or paranoid without clear reason.
- Increased tolerance, needing more of the substance to achieve the desired effect.
- Experiencing withdrawal symptoms when not using the substance.
- Neglecting responsibilities or hobbies.
- Loss of control over substance use (using more or longer than intended).
- Physical Signs:
- Bloodshot eyes, dilated pupils, or other unusual eye characteristics.
- Sudden weight changes (gain or loss).
- Poor personal hygiene or overall appearance.
- Unusual smells on breath, body, or clothing.
- Tremors, slurred speech, or impaired coordination.
- Social Signs:
- A sudden change in friends or social circles.
- Experiencing legal problems related to substance use.
- Financial difficulties, often unexplained.
- Continuing to use substances despite them causing relationship problems.
If you recognize these signs in yourself or a loved one, it might be time to seek Substance Use Support.
Signs of a Co-Occurring Mental Health Disorder
When a mental health disorder co-occurs with substance use, its signs can be exacerbated or masked. Look out for:
- Sudden or severe mood swings: Beyond typical emotional reactions.
- Social withdrawal: Isolating from friends, family, and activities once enjoyed.
- Significant changes in sleep or appetite: Insomnia, excessive sleeping, overeating, or loss of appetite.
- Extreme anxiety or paranoia: Persistent worry, panic attacks, or unfounded suspiciousness.
- Delusional thinking: Believing things that are not real or logical.
- Suicidal thoughts or self-harming behaviors: This is a critical warning sign and requires immediate attention.
If you or someone you know is experiencing a Mental Health Crisis or having thoughts of suicide, please call or text the 988 Suicide & Crisis Lifeline at 988 immediately. In life-threatening situations, always call 911.
The Path to Recovery: Integrated Treatment for Mental Health and Substance Use Co-Occurring Disorders
For individuals struggling with mental health and substance use co occurring disorders, the most effective path to recovery is an integrated treatment approach. This means addressing both conditions at the same time, in a coordinated manner, by the same treatment team or provider.
Why is an Integrated Approach So Important?
Historically, treatment for co-occurring disorders often followed a “sequential” model: treat the substance use first, then the mental health issue, or vice versa. This approach frequently failed because:
- Interference: Untreated mental health symptoms could trigger relapse into substance use. Conversely, active substance use could make mental health treatment ineffective.
- Incomplete Healing: Treating only one part of the problem left the other unaddressed, creating a revolving door of symptoms and treatment attempts.
Integrated treatment recognizes that these conditions are intertwined and must be tackled simultaneously. It provides comprehensive care that stabilizes both the symptoms of the mental health disorder and the substance use disorder, laying a stronger foundation for lasting recovery. This ensures that treatment is holistic and custom to the individual’s unique needs, recognizing that each person’s journey is different.
At SoberSteps, we understand the critical need for integrated care. We offer resources to help you find appropriate Co-occurring Disorders Treatment options. Taking this step is a sign of incredible strength. Don’t hesitate to Find Addiction Treatment that addresses all aspects of your well-being.
The Role of Behavioral Therapies
Behavioral therapies are a cornerstone of integrated treatment for co-occurring disorders. They help individuals develop coping skills, change unhealthy thought patterns, and build a supportive lifestyle. Some key therapies include:
- Cognitive Behavioral Therapy (CBT): This therapy helps individuals identify and change negative thought patterns and behaviors that contribute to both substance use and mental health symptoms. It teaches practical strategies for managing triggers and developing healthier responses. Learn more about Cognitive Behavioral Therapy.
- Dialectical Behavior Therapy (DBT): Often used for individuals with intense emotional dysregulation, DBT focuses on teaching skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. It’s particularly effective for those with co-occurring borderline personality disorder or severe mood disorders. Explore Dialectical Behavior Therapy.
- Motivational Interviewing: This client-centered approach helps individuals explore and resolve their ambivalence about change, fostering intrinsic motivation for recovery.
- Contingency Management: This therapy uses incentives and rewards to encourage positive behaviors, such as abstinence from substances or adherence to treatment goals.
These therapies are vital for building resilience, improving communication, and developing healthy ways to steer life’s challenges without resorting to substance use.
Medications in Dual Diagnosis Treatment
Medication can play a crucial role in managing the symptoms of both mental health disorders and substance use disorders, especially when used under careful medical supervision.
- Managing Mental Health Symptoms: Medications like antidepressants, mood stabilizers, or anti-anxiety medications can significantly reduce the severity of mental health symptoms, making it easier for individuals to engage in therapy and focus on recovery.
- Reducing Cravings and Withdrawal: For substance use disorders, certain medications can help reduce cravings for drugs or alcohol and ease uncomfortable withdrawal symptoms. This is often referred to as Medication-Assisted Treatment (MAT). For example, there is important Information on Medications for Opioid Use Disorder that can be life-changing for many.
- Non-Addictive Medications: Many medications used for mental health conditions are non-addictive, providing relief without creating new dependencies.
- Importance of Medical Supervision: It’s critical that all medications are prescribed and monitored by a qualified healthcare professional to ensure safety, effectiveness, and to manage any potential side effects or interactions.
Combining medication with behavioral therapies often yields the most successful outcomes for mental health and substance use co occurring disorders. If you’re struggling with cravings, seeking Help With Cravings can provide valuable support.
Levels of Care for Co-Occurring Disorders
Treatment for mental health and substance use co occurring disorders is not a one-size-fits-all solution; it’s a continuum of care custom to an individual’s needs. Understanding the different Levels of Care can help you determine the best starting point:
- Medical Detox: This is often the first step, especially for severe substance dependencies. Medical detox provides a safe, supervised environment to manage withdrawal symptoms, which can be dangerous and uncomfortable. During this phase, medical professionals can also begin to stabilize acute mental health symptoms.
- Inpatient/Residential Rehab: For individuals requiring a highly structured and supportive environment, residential treatment offers 24/7 care. This setting allows for intensive therapy, medication management, and a focus on both mental health and substance use recovery away from external triggers. Explore options for Inpatient Drug Rehab.
- Partial Hospitalization Program (PHP): PHPs offer a step down from residential care or a more intensive alternative to outpatient. Patients attend treatment for several hours a day, multiple days a week, but return home in the evenings. This allows for significant therapeutic engagement while maintaining some independence.
- Intensive Outpatient Program (IOP): IOPs provide structured therapy and support several times a week, for a few hours per session. This level of care is suitable for those who need significant support but can manage daily responsibilities and live at home.
- Outpatient and Aftercare: This is the least intensive level of care, offering ongoing therapy, support groups, and medication management appointments. Aftercare planning is crucial for long-term recovery, providing continued support as individuals transition back to their daily lives.
The goal is to find the right level of support that matches the severity of both the mental health and substance use conditions, ensuring a stable and sustainable recovery journey.
Finding Help and Supporting a Loved One
The journey of recovery from mental health and substance use co occurring disorders is rarely traveled alone. The support of family and a strong community can make a profound difference.
The Family’s Role in Recovery
Families are often deeply affected by co-occurring disorders, and their involvement can be a powerful force for healing. Here’s how families can support recovery:
- Education: Learning about both the mental health disorder and the substance use disorder helps family members understand the challenges their loved one faces and reduces stigma. Knowledge empowers families to react constructively rather than with blame or frustration.
- Setting Healthy Boundaries: This is crucial for both the individual in recovery and the family’s well-being. Boundaries protect against enabling behaviors and create a framework for mutual respect and accountability.
- Communication: Open, honest, and compassionate communication can strengthen family bonds and provide a supportive environment. Family therapy can be an excellent tool for improving communication patterns.
- Self-Care for Family Members: Supporting a loved one with co-occurring disorders can be emotionally taxing. It’s essential for family members to prioritize their own mental and physical health, seeking support groups or therapy for themselves.
- Avoiding Enabling: While well-intentioned, enabling behaviors can inadvertently hinder recovery. Learning to differentiate between support and enabling is a vital step for families.
For comprehensive guidance and support, families can find valuable Resources for Families Coping with Mental and Substance Use Disorders.
Where to Find Professional Help for Mental Health and Substance Use Co Occurring Disorders
Taking the first step to seek help can feel overwhelming, but we are here to guide you. Finding the right professional support is crucial for mental health and substance use co occurring disorders:
- Starting with Your Doctor: Your primary care physician can be an excellent first point of contact. They can conduct initial screenings, offer referrals to mental health specialists or addiction treatment centers, and help coordinate care.
- Using Treatment Locators: Several federal resources can help you find qualified treatment providers. SAMHSA’s National Helpline (1-800-662-HELP (4357)) and their online FindTreatment.gov tool are invaluable for locating facilities and providers in your area.
- Verifying Insurance: Understanding your insurance coverage is an important step. Many insurance plans, including Medicaid, now cover both mental health and substance abuse treatment. You can learn more with our Mental Health Insurance Complete Guide. SoberSteps also helps you Verify Insurance to understand your benefits.
You don’t have to steer this alone. We provide resources on How to Find Rehab and encourage you to Get Help Now if you or a loved one needs support.
The Power of Peer Support for Mental Health and Substance Use Co Occurring Disorders
Beyond professional treatment, peer support groups offer an invaluable layer of understanding, encouragement, and shared experience for individuals managing mental health and substance use co occurring disorders. These groups provide a safe space where individuals can connect with others who truly understand their struggles.
Some notable peer support groups include:
- Dual Recovery Anonymous (DRA): Specifically designed for individuals recovering from both chemical dependency and a mental health disorder, DRA offers a 12-step program custom to this unique challenge. Dual Recovery Anonymous is a fantastic resource.
- Alcoholics Anonymous (AA): While primarily focused on alcohol addiction, many AA groups are welcoming and understanding of co-occurring mental health issues.
- Narcotics Anonymous (NA): Similar to AA, NA provides a 12-step framework for recovery from drug addiction.
- SMART Recovery: This program focuses on self-empowerment and self-reliance, using a science-based approach to help individuals manage their addictions and related problems.
Finding a community of peers who share similar experiences can combat feelings of isolation, provide practical advice, and offer a powerful sense of belonging, which is crucial for long-term recovery.
Frequently Asked Questions about Co-Occurring Disorders
We know you might have more questions about mental health and substance use co occurring disorders. Here are some common ones we encounter:
What is the difference between dual diagnosis and co-occurring disorders?
The terms “dual diagnosis” and “co-occurring disorders” are often used interchangeably to describe the same condition: when an individual has both a substance use disorder and a mental health disorder at the same time. “Dual diagnosis” is an older term that is still widely used and understood, while “co-occurring disorders” has become the preferred and more clinically precise term. Regardless of the terminology, both refer to the critical need to address both conditions simultaneously for effective treatment.
Can you fully recover from co-occurring disorders?
Yes, absolutely. Recovery from mental health and substance use co occurring disorders is a very real and achievable goal. While it’s often described as a lifelong journey rather than a “cure,” it is entirely possible to manage both conditions effectively and live a fulfilling, productive life. With integrated treatment, ongoing support, and personal commitment, individuals can learn coping strategies, maintain sobriety, and improve their mental well-being. Success in managing these conditions is about developing resilience and a strong support system. A key component of this journey is developing effective Relapse Prevention strategies to steer challenges.
How do I pay for co-occurring disorder treatment?
Concern about the cost of treatment is very common, but there are many options available.
- Insurance Coverage: Most private insurance plans, as well as public programs like Medicaid, are mandated to cover mental health and substance abuse treatment. The extent of coverage can vary, so it’s important to verify your specific benefits.
- State-Funded Programs: Many states offer publicly funded treatment programs or financial assistance for those who qualify, especially for individuals with limited income or no insurance.
- Payment Plans and Sliding Scales: Many treatment facilities offer payment plans, financing options, or sliding scale fees based on income to make treatment more accessible.
Don’t let financial concerns prevent you from seeking help. We provide resources to help you understand How Do I Pay For Addiction Treatment and can assist with Verify Insurance inquiries to clarify your coverage.
Conclusion: Taking the First Step Towards Integrated Healing
The journey to recovery from mental health and substance use co occurring disorders can feel daunting, but hope is not lost. We’ve explored the intricate connections between these conditions, from shared risk factors and brain chemistry to the complex ways they influence each other. We’ve also highlighted the critical importance of integrated treatment, which addresses both conditions simultaneously, and the diverse range of therapies and support systems available.
Seeking help is not a weakness; it’s a profound act of strength and self-care. If you or a loved one is struggling, know that you are not alone, and effective treatment is within reach.
SoberSteps is an independent resource dedicated to helping you explore confidential Co-occurring Disorders Treatment options and understand the path to recovery. Your healing journey starts with a single step, and we’re here to guide you along the way.



