Understanding Your Path to Recovery
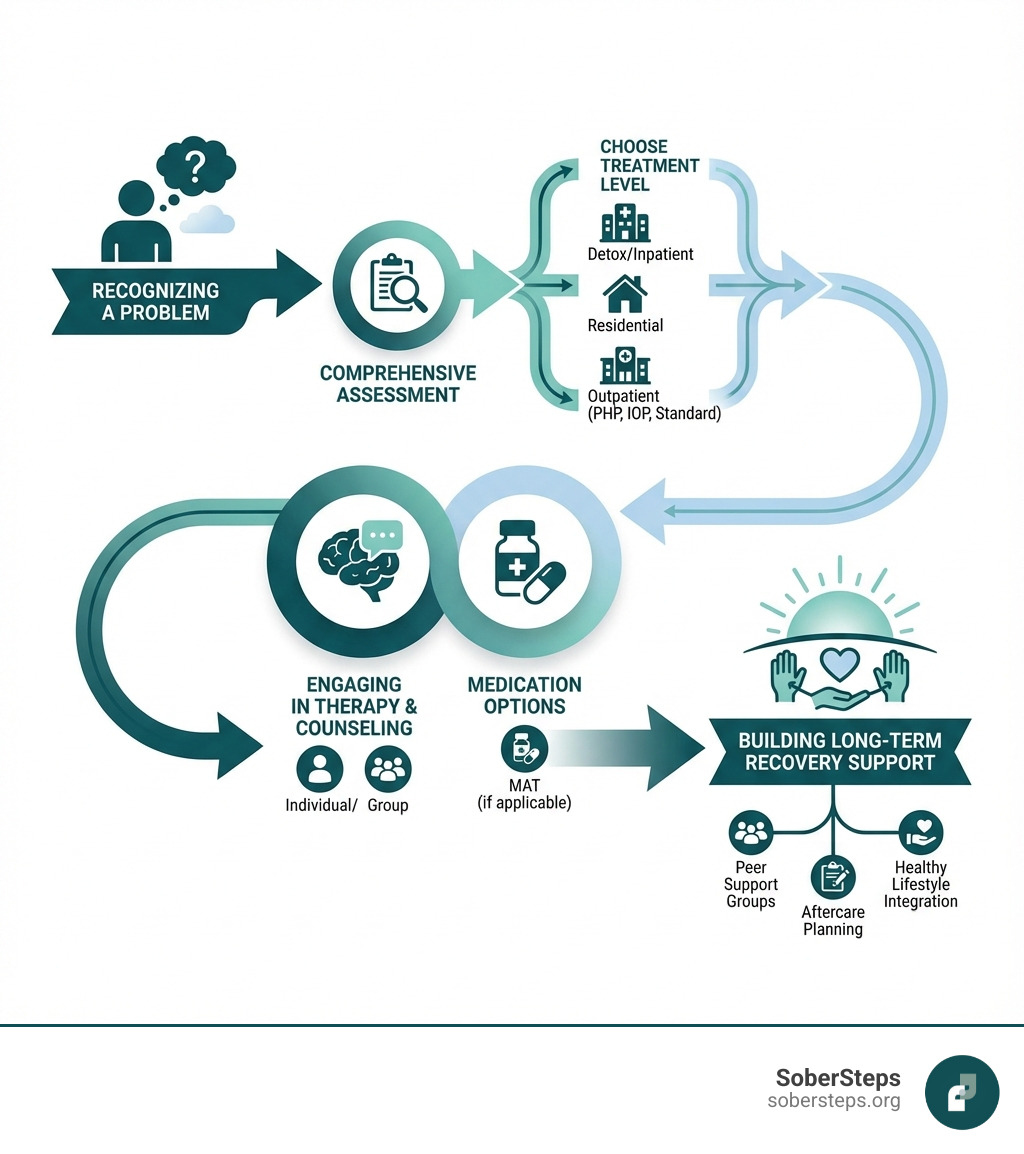
A treatment options guide is essential for anyone facing addiction or mental health challenges. It helps you understand the different types of care available, from medical detox to outpatient therapy, and guides you toward the right support for your unique situation. Here’s what you need to know:
Key Components of a Treatment Options Guide:
- Levels of Care – Medical detox, inpatient rehab, residential programs, partial hospitalization (PHP), intensive outpatient (IOP), standard outpatient, and telehealth options
- Therapeutic Approaches – Individual therapy, group counseling, cognitive behavioral therapy (CBT), family therapy, and peer support groups
- Medication-Assisted Treatment – FDA-approved medications for alcohol and opioid use disorders, combined with counseling
- Payment Options – Insurance coverage, sliding scale fees, government programs, and patient assistance
- Professional Support – Working with therapists, counselors, psychiatrists, and case managers who guide your recovery
If you’re feeling overwhelmed by the choices ahead, you’re not alone. In 2022, more than one in six Americans aged 12 or older experienced a substance use disorder. Many of them faced the same questions you might be asking now: Where do I start? What kind of treatment do I need? How do I pay for it?
The reality is that treatment is not one-size-fits-all. What works for one person may not be the best fit for another. That’s why understanding your options is so crucial.
A comprehensive treatment options guide empowers you to make informed decisions, reduces stigma, and clarifies what to expect during treatment. Whether you’re seeking help for yourself or a loved one, this guide clarifies the path forward. Recovery is possible, and it starts with understanding your options.
At Sober Steps, our mission is to provide the reliable, confidential information you need to steer addiction treatment. Our comprehensive guide and support resources have helped countless individuals and families take the first steps toward recovery.
Ready to explore your options? Get Help Now or continue reading to learn about the full spectrum of care available to you. If you need immediate support, our confidential helpline is available to answer your questions and connect you with the right resources.
Exploring the Spectrum of Care: Types of Treatment Options
This section breaks down the various modalities and settings available for treatment, helping you understand what might be the best fit for your unique situation. Finding the right combination of care is the first step toward recovery.
Levels of Care: From Detox to Outpatient
Understanding the different levels of care is crucial when navigating your treatment options guide. The right level for you depends on the severity of your condition, your physical and mental health, and your living environment.
-
Medical Detox: The first step for physical dependence on substances like alcohol or opioids. It’s a medically supervised process to manage withdrawal symptoms safely, preparing you for further treatment. If you need immediate help, explore options for Detox Near Me.
-
Inpatient Rehabilitation: Provides 24/7 support in a structured environment, ideal for focusing entirely on recovery away from daily triggers. Programs typically last 30-90 days and offer immersive therapeutic activities. Learn more about Inpatient Drug Rehab.
-
Residential Treatment: Offers live-in care similar to inpatient rehab but for longer durations (one month to a year or more). It’s beneficial for those needing a stable environment for long-term, phased treatment.
-
Partial Hospitalization Programs (PHP): Offers intensive outpatient services (25-30 hours per week) while you return home each evening. PHP is a step-down from inpatient care for those with a stable home environment.
-
Intensive Outpatient Programs (IOP): A flexible option with 9-15 hours of therapy per week, allowing you to maintain work or school responsibilities. IOPs offer day and evening schedules and typically last 8-12 weeks.
-
Standard Outpatient: Involves regular counseling sessions while living at home. It’s suitable for those with stability in recovery who need ongoing support and relapse prevention strategies.
-
Telehealth options: Provides treatment online or by phone, making care accessible for those with location, mobility, or scheduling conflicts.
You can find more detailed information on these levels of care in our dedicated section: More info about Levels of Care.
Therapeutic Modalities and Counseling

Therapy and counseling are cornerstones of any effective treatment options guide. These approaches help you understand the root causes of your struggles and develop healthy coping mechanisms.
-
Psychotherapy: Also known as “talk therapy,” it involves speaking with a therapist in a safe environment to explore feelings and behaviors and gain skills to manage life’s challenges.
-
Cognitive Behavioral Therapy (CBT): A widely used therapy that focuses on the connection between thoughts, feelings, and behaviors. CBT teaches you to identify and change negative thought patterns that contribute to addiction or mental health issues.
-
Dialectical Behavior Therapy (DBT): A form of CBT that teaches skills in emotional regulation, mindfulness, and interpersonal effectiveness. It’s helpful for those with intense emotions and self-destructive behaviors.
-
Motivational Interviewing: A client-centered approach that helps you resolve ambivalence about change by guiding you to find your own motivation for recovery.
-
Family and couples counseling: Involves loved ones to improve communication, address family dynamics, and build a supportive environment for recovery. Involving family is a key part of effective treatment.
-
Group therapy benefits: Connects you with peers who have similar experiences, reducing isolation and fostering a sense of community and shared understanding.
-
Peer support: Connects you with individuals who have lived experience in recovery, offering invaluable empathy, encouragement, and practical advice.
To dive deeper into these and other therapeutic approaches, visit our page on Explore different types of Therapy.
Medication-Assisted Treatment (MAT)
Medication-Assisted Treatment (MAT) is a vital part of many treatment options guide plans, especially for opioid and alcohol use disorders. MAT combines FDA-approved medications with counseling to treat the whole person. The medications work to normalize brain chemistry, relieve cravings, and manage withdrawal symptoms, making recovery more manageable. The counseling component is just as important as the medication.
-
Medications for Alcohol Use Disorder (AUD): Three FDA-approved medications help prevent relapse:
- Naltrexone: Blocks the rewarding effects of alcohol. Available as a daily pill or monthly injection.
- Acamprosate: Eases emotional discomfort like anxiety and restlessness during early abstinence.
- Disulfiram: Causes unpleasant symptoms if alcohol is consumed, acting as a deterrent.
Despite their effectiveness, a 2021 analysis found these medications are vastly underused, prescribed to only 1.6% of adults with AUD.
-
Medications for Opioid Use Disorder (MOUD): There are three FDA-approved medications:
- Buprenorphine: Controls withdrawal and cravings and can be prescribed in an office setting.
- Methadone: Reduces cravings and withdrawal, dispensed at licensed Opioid Treatment Programs (OTPs).
- Naltrexone: Blocks the effects of opioids, removing their rewarding properties.
You can learn more about these critical medications at Medication-Assisted Treatment (MAT) | SAMHSA.
-
Reducing cravings and withdrawal: The primary goal of these medications is to make recovery more manageable by alleviating the intense physical discomfort and psychological cravings that often lead to relapse.
A Comprehensive Treatment Options Guide: Key Components for Success
A good treatment plan is more than just a single solution; it’s a personalized roadmap. This comprehensive treatment options guide highlights the essential elements that contribute to effective and lasting recovery.
The Importance of Evidence-Based Practices

When exploring your treatment options guide, prioritize “evidence-based practices”—treatments proven effective through scientific research. These approaches, recommended in clinical guidelines, ensure you receive care that works.
-
Proven effectiveness: Choosing evidence-based treatments increases your chances of success. For example, Medications for Opioid Use Disorder (MOUD) are proven to reduce illicit opioid use, increase treatment retention, and decrease overdose risk. Similarly, SSRIs are a first-line treatment for OCD, though they often require higher doses for this condition compared to depression.
-
Ensuring quality of care: Quality programs prioritize these practices, are licensed and accredited, and employ specially trained staff. This commitment ensures you receive the highest standard of care.
For more information on treatments backed by solid research, you can Learn more about evidence-based treatments from NAMI.
Personalizing Your Treatment Path: A Guide to Individual Needs
A core principle of any treatment options guide is that recovery is not “one-size-fits-all.” Your treatment plan must be personalized to your unique needs and circumstances.
-
Biopsychosocial assessment: Clinicians conduct a comprehensive assessment of your biological, psychological, and social factors to create a personalized plan.
-
ASAM Criteria: These criteria help clinicians match you to the right level of care by evaluating six dimensions of your life, from withdrawal risk to your recovery environment.
-
Co-occurring disorders: About half of people with a substance use disorder also have a mental health condition. Integrated Dual Diagnosis treatment addresses both simultaneously and is essential for long-term recovery.
-
Personal factors: A good plan also considers your personal history, trauma, cultural background, and individual preferences (e.g., individual vs. group therapy, telehealth needs).
If you’re ready to find a program that truly fits your unique needs, don’t hesitate to Find a program that fits your needs.
Focusing on Long-Term Recovery and Relapse Prevention
An effective treatment options guide looks beyond initial treatment to focus on lifelong recovery and relapse prevention.
-
Recovery as a lifelong journey: Addiction and mental health conditions are often chronic and require ongoing management, similar to diabetes or heart disease.
-
Aftercare planning: A crucial step is creating a strategy for continued support after leaving an intensive program. This may include ongoing therapy or case management.
-
Sober living environments: These transitional homes provide a structured, substance-free environment that bridges the gap between intensive treatment and independent living.
-
Support groups (12-step, SMART Recovery): Groups like AA, NA, SMART Recovery, and others offer invaluable peer connection, accountability, and shared wisdom.
-
Building coping skills: Therapy equips you with tools to manage triggers, stress, and difficult emotions without returning to unhealthy behaviors.
-
Creating a support network: Surrounding yourself with supportive family, friends, and peers is fundamental to long-term success.
For comprehensive strategies, explore our Relapse Prevention strategies. We also invite you to Read inspiring Addiction Success Stories to see that long-term recovery is truly possible.
Navigating the Practicalities: Paying for Treatment
The financial aspect of treatment can be a major concern, but numerous options are available. Understanding how to pay for care can remove a significant barrier to getting the help you need.
Understanding Your Payment Options
Worrying about cost shouldn’t be a barrier to getting help. A good treatment options guide clarifies the various ways to pay for care.
-
Health insurance plans: Most insurance plans cover addiction and mental health treatment. Parity laws ensure this coverage is comparable to medical benefits.
-
Private pay: Paying out-of-pocket is an option, and many facilities offer payment plans.
-
Sliding scale fees: Non-profit centers often adjust costs based on your income.
-
Government-funded programs: Federal and state programs offer financial assistance for those with limited income. SAMHSA’s FindTreatment.gov can help you locate them.
-
Grants and scholarships: Non-profits and some treatment centers offer financial awards to help cover costs.
To get a full picture of the financial landscape, refer to our guide on How Do I Pay for Addiction Treatment?.
How to Verify Insurance and Access Help
Understanding your insurance benefits for addiction and mental health treatment can feel like navigating a maze. Our treatment options guide aims to simplify this process, so you can confidently access the care you deserve.
-
Contacting your insurance provider: The first step is to call your insurance company to get details on your plan’s coverage, including deductibles, co-pays, and in-network providers.
-
Understanding your benefits: Ask about your out-of-pocket maximum and any limits on therapy sessions or length of stay.
-
Parity laws: The Mental Health Parity and Addiction Equity Act (MHPAEA) requires most plans to cover mental health and addiction treatment equally with medical care. You can find robust resources and support on this topic from Mental Health and Addiction Insurance Help (HHS).
-
Patient assistance programs: Pharmaceutical companies and other organizations may offer programs to help lower the cost of medications.
To make this step easier, we offer a straightforward way for you to Verify your insurance coverage with us today. This can give you clarity on your benefits and help you plan your treatment journey without financial surprises.
Building Your Support System: The Role of Professionals and Shared Decision-Making
You are not alone in this process. A team of dedicated professionals and your own active involvement are crucial for creating a successful treatment plan.
Working with Your Healthcare Team
A comprehensive treatment options guide emphasizes the importance of a collaborative healthcare team. Together, they form a powerful support system.
-
Primary care physicians: Your doctor can be a first point of contact for screening, brief counseling, and referrals to specialists.
-
Therapists and counselors: These licensed professionals provide psychotherapy to help you develop coping skills and address underlying issues.
-
Psychiatrists: As medical doctors, they diagnose conditions and manage psychiatric medications.
-
Case managers: These professionals help coordinate your care and connect you with resources.
-
Addiction specialists: These experts have specific training in treating substance use disorders.
-
The importance of a collaborative approach: The most effective plans involve these professionals working together to tailor care to your needs.
To build the right team for your recovery, start by exploring how to Find the right Substance Abuse Treatment team.
Shared Decision-Making: Your Voice in Your Care
At the heart of an empowering treatment options guide is the principle of shared decision-making. This means you are an active, informed participant in all aspects of your treatment.
-
Patient empowerment: You are the expert on your own life. We empower you to voice your preferences and help design your recovery plan.
-
Asking questions: Don’t hesitate to ask your team about the benefits, risks, and alternatives for any proposed treatment.
-
Understanding risks and benefits: Ethical healthcare practice requires professionals to inform you of all reasonable options so you can make an informed choice.
-
Defining your own recovery goals: Your personal wellness and recovery goals should guide your treatment plan.
-
Being an active participant in your treatment plan: Your involvement—attending sessions, communicating openly, and providing feedback—directly impacts your success.
-
Professional ethical duty to inform patients: Healthcare providers are ethically obliged to involve patients in treatment decisions. This principle is central to quality care in all medical fields, including addiction and mental health.
Ready to take control of your recovery journey and make your voice heard? Get Help Now and take control of your recovery.
Frequently Asked Questions about Choosing a Treatment Option
How do I know which level of care is right for me?
The right level of care depends on factors like the severity of the substance use, physical health, mental health status, and home environment. A professional assessment, often using tools like the ASAM Criteria, is the best way to determine whether inpatient or outpatient care is most appropriate. These assessments consider how much support you need, your risk of withdrawal, and your overall well-being.
What is the difference between therapy and medication-assisted treatment (MAT)?
Therapy addresses the psychological and behavioral aspects of addiction, helping you develop coping skills, understand triggers, and change thought patterns. MAT uses FDA-approved medications, in combination with counseling, to treat the physiological aspects, such as withdrawal symptoms and intense cravings. Many successful treatment plans incorporate both therapy and MAT for a holistic approach.
How long does treatment last?
Treatment duration is highly individualized and is not a fixed timeline. It can range from a 30-day inpatient program to several months or years of outpatient support and aftercare. The goal is to provide enough support to ensure a stable foundation for long-term recovery, with the understanding that recovery is often measured in months, not just days or weeks.
Conclusion
Navigating recovery can feel complex, but this treatment options guide is designed to simplify the process and empower you with knowledge. From understanding different drug treatment options to paying for care and building a support system, the path to a healthier life is achievable. Recovery is a journey, not a destination, and taking the first step is the most important part. SoberSteps is here to help you on that path with resources and a confidential helpline. Explore our complete guide to drug treatment programs or call us today to get started.



