
Why Opioid Rehab is Essential for Recovery
Opioid rehab is a comprehensive treatment approach that combines medical detox, medications, counseling, and support services to help individuals overcome opioid addiction and rebuild their lives. If you or someone you love is struggling with opioid use disorder (OUD), here’s what you need to know:
Key Treatment Options Available:
- Medical Detox – Supervised withdrawal management in a safe environment
- Medication-Assisted Treatment (MAT) – FDA-approved medications (buprenorphine, methadone, naltrexone) combined with therapy
- Inpatient Rehab – 24/7 residential care with structured programming (30-90 days)
- Outpatient Programs – Flexible treatment while living at home (IOP, PHP)
- Behavioral Therapy – Individual and group counseling to address underlying issues
- Aftercare Support – Ongoing recovery resources and relapse prevention
Opioid use disorder is a chronic disease that affects millions of Americans. The good news? Recovery is absolutely possible. Research shows that medication treatment of OUD reduces the risk of overdose and overall mortality. Treatment works by normalizing brain chemistry, relieving cravings, and helping you regain control of your life.
The journey can feel overwhelming, especially when you’re trying to understand diagnostic criteria, treatment settings, medication options, and how to pay for care. You might be wondering: How long does rehab take? What happens during detox? Will my insurance cover it? These are all valid questions—and we’re here to help you find answers.
At Sober Steps, we’ve been guiding individuals and families through the opioid rehab process for years, connecting them with quality treatment resources and providing the support they need to start their recovery journey. We understand that choosing the right treatment path is deeply personal, and we’re committed to helping you find options that fit your unique situation.
If you or a loved one is struggling, contact SoberSteps today for confidential help.
Learn more about our approach to recovery.
Understanding Opioid Use Disorder and Why Rehab is Crucial
Opioid addiction, also known as opioid use disorder (OUD), is a chronic and relapsing disease that can affect anyone. It’s a complex condition, not a moral failing, and it requires a comprehensive, evidence-based approach to treatment. At SoberSteps, we believe that lasting recovery takes more than hope; it takes science and dedicated care.
What is Opioid Addiction?
Opioid addiction, or OUD, is characterized by the compulsive use of opioids despite the clinically significant impairment it causes to one’s life. Opioids are powerful substances that hijack the brain’s dopamine reward system, creating an intense desire to repeat drug use. This interaction can explain why opioid drugs have such undesired and powerful effects. When someone develops OUD, their brain chemistry changes, leading to physical dependence and severe withdrawal symptoms if they try to stop. This makes seeking professional help through opioid rehab not just beneficial, but often life-saving.
We approach addiction as a disease, similar to diabetes or heart disease, that requires ongoing management and treatment. Learn more about addiction as a disease and dig deeper into Opioid Addiction. If you’re unsure whether you or a loved one might be struggling, you can take our self-assessment to gain clarity. It’s an important first step toward recognizing the problem and finding the right help. To understand more about the indicators, you can also recognize the signs of addiction.
Commonly Misused Opioids
Opioids encompass a wide range of substances, both legal and illicit, that share a similar chemical structure and effect on the brain. These include natural opiates derived from the poppy plant, semi-synthetic opioids, and fully synthetic opioids. When prescribed correctly, opioids can effectively manage pain. However, their euphoric effects make them highly susceptible to misuse and addiction.
Here are some of the commonly misused opioids we encounter in opioid rehab:
- Prescription Painkillers: These include drugs like Oxycodone (often found in OxyContin and Percocet), Hydrocodone (Vicodin), and Morphine. These are powerful pain relievers that can quickly lead to physical and psychological dependence, even when initially used as prescribed.
- Illicit Drugs: Heroin is a well-known illicit opioid that is often injected, snorted, or smoked. It’s highly addictive and carries significant risks due to its unknown purity and potency.
- Potent Synthetic Opioids: Fentanyl is a synthetic opioid that is 50 to 100 times more potent than morphine. While it has legitimate medical uses for severe pain, illegally manufactured fentanyl is frequently abused and is a major contributor to overdose deaths in the U.S.
Understanding these different types of opioids is crucial for effective treatment. We offer guidance on various substance use disorders; you can see our guide to commonly misused drugs for more information.
Signs and Symptoms of Opioid Use Disorder
Recognizing the signs of OUD is the first step toward seeking help. The diagnostic criteria for OUD, based on the DSM-5, require an individual to exhibit at least two of 11 symptoms within a 12-month period. These symptoms cover a spectrum of behavioral, physical, and psychological changes.
Behavioral Signs:
- Taking opioids in larger amounts or over a longer period than intended.
- A persistent desire or unsuccessful efforts to cut down or control opioid use.
- Spending a great deal of time obtaining, using, or recovering from the effects of opioids.
- Craving, or a strong desire or urge to use opioids.
- Failure to fulfill major role obligations at work, school, or home due to opioid use.
- Continuing opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of opioids.
- Giving up important social, occupational, or recreational activities because of opioid use.
- Recurrent opioid use in situations in which it is physically hazardous.
- Continuing opioid use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by opioids.
- “Doctor shopping”: Seeking multiple prescriptions from different clinicians to obtain more opioids is a common red flag.
Physical Signs:
- Tolerance: A need for markedly increased amounts of opioids to achieve intoxication or desired effect, or a markedly diminished effect with continued use of the same amount of an opioid.
- Withdrawal: A characteristic opioid withdrawal syndrome (see below), or opioids are taken to relieve or avoid withdrawal symptoms.
- Pinpoint Pupils: Very small pupils are a common sign of opioid influence.
- Constipation and Nausea: These are two of the most common side effects of opioid use.
- Risk of Falls: Opioids increase the risk and incidence of falls, leading to severe injuries.
Psychological Signs:
- Mood swings, anxiety, and depression are often observed. People with underlying mental health concerns are at higher risk of developing OUD.
- Opioids can interfere with the immune response, making individuals more vulnerable to illnesses.
- Long-term opioid use can lead to hyperalgesia, a heightened pain sensitivity, paradoxically making pain worse.
Experiencing Drug Withdrawal is a significant indicator of physical dependence. The symptoms can be severe and include nausea, vomiting, anxiety, insomnia, hot and cold flushes, perspiration, muscle cramps, watery eyes and nose, and diarrhea. These symptoms can appear within hours of the last dose.
If these signs resonate with your experience or that of a loved one, it’s crucial to seek professional assessment. You can find more details to recognize the signs of addiction. For a confidential discussion about these symptoms and next steps, please contact us for a confidential assessment.
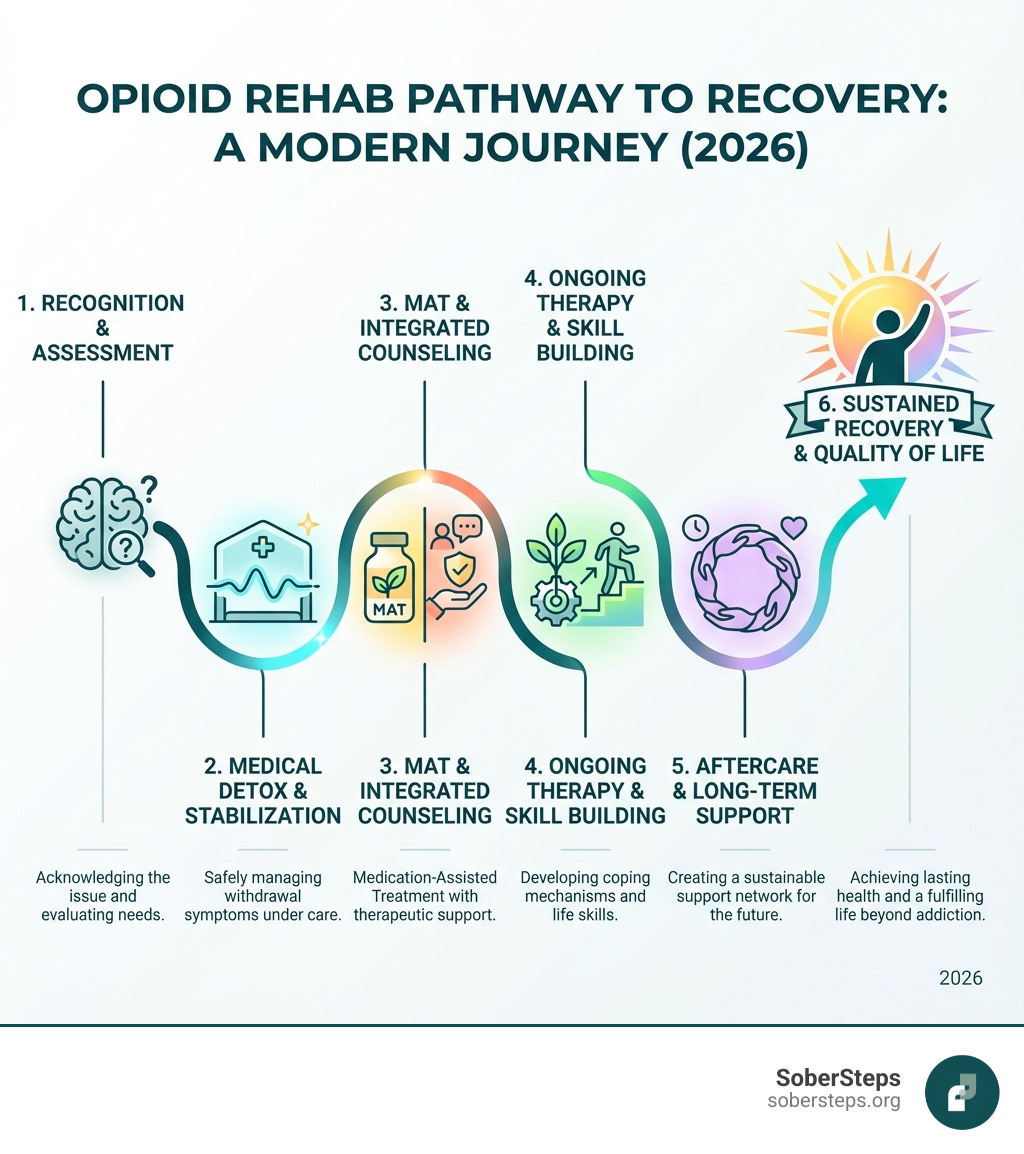
What to Expect from the Opioid Rehab Process
Starting on the journey of opioid rehab can feel daunting, but understanding the process can empower you to take those crucial first steps. Our approach is designed to guide individuals through each stage of recovery, providing support and expert care every step of the way.
The First Step: Medically Supervised Detox
For most individuals with OUD, the first and often most challenging step in opioid rehab is detoxification. This process focuses on safely removing opioids from the body and managing the often painful and uncomfortable withdrawal symptoms. Medically supervised detox is highly recommended for opioid use disorders because withdrawal symptoms can be severe and dangerous, including intense cravings that can lead to immediate relapse and overdose.
During detox, medical professionals provide around-the-clock care, monitoring vital signs and administering medications to alleviate withdrawal symptoms. This ensures comfort and safety, preventing complications. For example, while outpatient detox might cost around $1,000 to $1,500, most inpatient rehabs include detox as part of their program cost, reflecting the comprehensive nature of this crucial initial phase.
It’s vital to understand that detoxification alone is generally not sufficient for long-term recovery. The CDC emphasizes that detox without medication for opioid use disorder is not recommended due to the increased risks for resuming drug use, overdose, and overdose death. It’s a necessary first step, but it must be followed by ongoing treatment to address the underlying behavioral and psychological aspects of addiction.
We offer comprehensive Inpatient Detox Program options to ensure a safe and stable start to recovery. To find immediate help or learn more, you can find a Detox Near Me or speak with our admissions team today. For more detailed information, please learn about our detox process.
Choosing the Right Level of Care for Opioid Rehab
Once detox is complete, the next critical step is transitioning into a structured treatment program. The American Society of Addiction Medicine (ASAM) outlines various levels of care, and choosing the right one is essential for effective opioid rehab. The best program for you or your loved one will depend on the severity of the addiction, co-occurring mental health conditions, and individual needs.

At SoberSteps, we offer a continuum of care designed to meet diverse needs:
- Inpatient Drug Rehab: Also known as residential treatment, this level of care provides 24/7 supervision and a highly structured environment. Patients live at the facility, allowing them to focus entirely on recovery away from triggers and temptations. These programs often last 30, 60, or 90 days. For instance, some inpatient rehabs may cost around $6,000 for a 30-day program, while well-known centers can be up to $20,000 for the same duration. Longer programs, typically 60 or 90 days, can range from $12,000 to $60,000.
- Outpatient Programs: These programs offer flexibility, allowing individuals to live at home while attending scheduled treatment sessions. They are suitable for those with strong support systems and less severe addiction.
- Partial Hospitalization Programs (PHPs): Often called “day treatment,” PHPs involve intensive therapy for several hours a day, typically 5 days a week (20 hours or more).
- Intensive Outpatient Programs (IOPs): IOPs provide structured treatment for 3 to 5 days a week, totaling at least 9 hours. Many outpatient programs cost around $5,000 for a three-month program, with some specialized programs reaching $10,000.
Research consistently shows that longer treatment durations yield better outcomes. Studies suggest that most people benefit from spending at least 90 days in treatment to effectively break habits and build new coping mechanisms. We encourage you to explore all Levels of Care to understand your options. You can also compare our treatment programs to find the best fit. If you’re feeling overwhelmed by choices, our team is here to help; get help choosing the right program.
Core Therapies and Long-Term Support
Effective opioid rehab extends beyond initial detox and medication. It digs into the psychological, emotional, and social factors contributing to addiction through evidence-based therapies and robust aftercare planning. Our goal is to equip individuals with the skills and support needed for lasting recovery.
Key therapeutic approaches we use include:
- Cognitive Behavioral Therapy (CBT): This therapy helps individuals identify and change negative thought patterns and behaviors that contribute to substance use. It provides practical strategies for coping with cravings and high-risk situations.
- Individual and Group Counseling: These sessions provide a safe space to explore personal challenges, develop self-awareness, and learn from the experiences of others in recovery.
- Family Therapy: Addiction affects the entire family system. Family therapy helps improve communication, heal relationships, and establish healthy boundaries, fostering a supportive environment for recovery.
Many individuals struggling with OUD also face co-occurring mental health issues like depression, anxiety, or PTSD. Addressing these conditions simultaneously is crucial for successful recovery. Our Dual Diagnosis Treatment ensures that both addiction and mental health challenges receive integrated care.
Aftercare planning is a critical component of opioid rehab. As the American Society of Addiction Medicine (ASAM) recommends, continued participation in counseling and support groups post-treatment is crucial for reinforcing new skills and improving long-term outcomes. This includes developing robust Relapse Prevention strategies to steer triggers and maintain sobriety. Aftercare services may involve ongoing therapy, peer support groups (like 12-step programs), sober living environments, and telehealth options for continued support.
Your recovery journey is unique, and we’re here to support you at every turn. Start your recovery journey now and learn about our therapy options.
Medication-Assisted Treatment (MAT) and Overdose Prevention
Medication-Assisted Treatment (MAT) is a cornerstone of modern opioid rehab, recognized by leading health organizations as the most effective approach for treating OUD. It’s a scientifically-backed strategy that significantly improves outcomes.
How MAT Supports Recovery in Opioid Rehab
MAT is a “whole-patient” approach that combines FDA-approved medications with counseling and behavioral therapies. This integrated strategy addresses the complex needs of individuals with OUD, tackling both the physical and psychological aspects of addiction. The National Institute on Drug Abuse (NIDA) highlights that MAT decreases opioid use and opioid-related deaths, while increasing social functioning and retention in treatment.
The medications used in MAT help to normalize brain chemistry, which has been altered by opioid use. They effectively relieve cravings and prevent severe withdrawal symptoms, allowing individuals to focus on their recovery journey without the constant struggle against physical dependence. This stability creates a foundation for engaging in therapy and developing essential coping skills.
MAT is not simply substituting one drug for another. It’s a carefully managed medical intervention that provides stability and support, enabling individuals to regain control of their lives. We provide comprehensive guidance and access to MAT as part of a holistic treatment plan. Learn about MAT at SoberSteps and take the vital step to get help now. If you have questions or want to explore if MAT is right for you, speak to a MAT specialist.
Overview of FDA-Approved Opioid Addiction Medications
The FDA has approved several medications specifically for the treatment of OUD, each working differently to support recovery. These medications are a critical component of MAT and are integrated into many opioid rehab programs.

-
Methadone:
- How it works: Methadone is a full opioid agonist. This means it binds to the same opioid receptors in the brain as other opioids but produces a milder, longer-lasting effect. It reduces opioid cravings and withdrawal symptoms without causing the euphoric “high” when taken as prescribed.
- Administration: Methadone is available as a daily liquid and must be dispensed through a SAMHSA-certified Opioid Treatment Program (OTP). Year-long methadone treatment for heroin users costs around $4,700, making it a cost-effective long-term solution.
- Role in Treatment: It helps stabilize individuals, allowing them to engage in counseling and rebuild their lives.
-
Buprenorphine:
- How it works: Buprenorphine is a partial opioid agonist. It binds to opioid receptors but produces a weaker effect than full agonists like methadone or heroin. It reduces cravings and withdrawal symptoms and can block the effects of other opioids, making them less rewarding. It’s often combined with naloxone (e.g., Suboxone) to prevent misuse.
- Administration: Buprenorphine is available as dissolving tablets, cheek films, injections (e.g., Sublocade), or implants (e.g., Probuphine). Unlike methadone, buprenorphine can be prescribed by any clinician with a standard DEA registration in various clinical settings, including a doctor’s office.
- Role in Treatment: It offers greater flexibility for patients and can be a good option for those seeking office-based treatment.
-
Naltrexone:
- How it works: Naltrexone is an opioid antagonist. It blocks opioid receptors, preventing any opioid from producing its euphoric or sedative effects. This makes opioid use pointless and eliminates the rewarding aspect of the drug.
- Administration: Naltrexone is available as an oral medication (ReVia, Depade) or a monthly extended-release injection (Vivitrol). It can be prescribed by any clinician with an active license.
- Role in Treatment: It’s typically started after an individual has been opioid-free for 7-10 days to avoid precipitating severe withdrawal. It’s an excellent option for preventing relapse once detox is complete.
Our team at SoberSteps can help you understand these options and integrate them into a comprehensive treatment plan. Learn more about medication options and don’t hesitate to ask about medication-assisted treatment when you reach out.
The Lifesaving Role of Naloxone (Narcan)
In the fight against the opioid crisis, one medication stands out as a true lifesaver: Naloxone, often known by its brand name Narcan. This medication is crucial for preventing fatal opioid overdoses and is an integral part of any comprehensive opioid rehab and overdose prevention strategy.
- How it works: Naloxone is an opioid antagonist that rapidly reverses the effects of an opioid overdose. When administered, it quickly binds to opioid receptors in the brain, knocking opioids off the receptors and restoring normal breathing. It can work within minutes, providing a critical window for medical help to arrive. The CDC recommends that anyone at risk of an opioid overdose or who knows someone struggling with opioid use disorder should carry Naloxone and keep it at home. In fact, a bystander is present in 40% of opioid and stimulant-involved overdose deaths, highlighting the need for increased public training and access to Naloxone.
- Good Samaritan Laws: To encourage individuals to act in an overdose emergency, many states have enacted Good Samaritan Laws. These laws typically protect both the person experiencing an overdose and the person seeking medical help for them from drug possession charges. This legal protection is vital because fear of legal repercussions can prevent people from calling 911 during an overdose, costing precious time.
- Accessing Naloxone: Naloxone is available in various forms, including nasal sprays and injectable solutions. It can often be obtained without a prescription from pharmacies in many states, through community programs, or by asking your doctor.
At SoberSteps, we believe in empowering individuals and communities with the knowledge and tools to prevent overdose fatalities. We can guide you on how to access Naloxone and provide training on its proper use. Learn about overdose prevention and request overdose prevention resources from our team.
Finding and Paying for Your Path to Recovery
Taking the step to seek opioid rehab is courageous, and we’re here to help you steer the practicalities, from finding the right facility to understanding how to cover the costs.
How to Find Quality Treatment Centers
Choosing a quality opioid rehab center is paramount for successful recovery. It’s not just about finding any facility; it’s about finding the right fit that offers evidence-based treatment and a supportive environment. When evaluating potential centers, we recommend looking for several key indicators:
- Accreditation and Licensing: Ensure the center is accredited by reputable organizations (e.g., The Joint Commission, CARF) and licensed by the state. This signifies adherence to high standards of care.
- Qualified Staff: Look for facilities with experienced and credentialed medical doctors, therapists, counselors, and support staff specializing in addiction medicine.
- Evidence-Based Treatment: Confirm that the center uses scientifically proven therapies and practices, such as MAT, CBT, and integrated care for co-occurring disorders.
- Individualized Treatment Plans: A one-size-fits-all approach rarely works. A good center will tailor a plan to your unique needs, history, and goals.
- Aftercare Planning: A strong aftercare program indicates a commitment to long-term recovery, not just initial treatment.
To assist you in this crucial search, we provide resources and tools. You can explore our guide on how to Find Rehab and use our Find Addiction Treatment tool for personalized help. For more detailed information or to discuss your options, please contact us for a free consultation. We’re also happy to walk you through our process; read about our admissions process.
Navigating Costs and Insurance Coverage
The cost of opioid rehab is a significant concern for many, but it shouldn’t be a barrier to seeking life-saving treatment. The good news is that various options exist to make treatment affordable. It’s also important to consider the long-term costs of untreated addiction, which can far outweigh the cost of rehab in terms of health problems, legal issues, lost income, and overall quality of life.
Costs for opioid rehab vary widely depending on several factors:
- Type of Center: Inpatient programs are generally more expensive than outpatient options due to 24/7 care, accommodation, and meals.
- Length of Program: Longer programs naturally incur higher costs. While a 30-day inpatient program might be around $6,000, 60- or 90-day programs can range from $12,000 to $60,000. Outpatient programs might cost $5,000 for three months.
- Treatments Offered: Specialized therapies, dual diagnosis treatment, and extensive medical care can influence the price.
- Amenities: Luxury facilities with extensive amenities will typically have higher price tags.
Understanding your insurance coverage is a critical step. Thanks to mental health parity laws, insurers are legally required to provide at least some coverage for addiction treatment. We can help you understand how Do I Pay For Addiction Treatment? and steer your Insurance options.
Medicare and Medicaid Coverage:
- Medicare: If you have Medicare, it covers many OUD treatment services. Medicare Part A may cover methadone in an inpatient hospital setting, while Part B covers methadone, buprenorphine, and naltrexone when provided through an Opioid Treatment Program (OTP). Medicare Part D may cover prescription medications like buprenorphine, naloxone, and naltrexone. Medicare also covers counseling and therapy, including virtual options. For services from a Medicare-enrolled OTP, there are often no copayments, though the Part B deductible might apply to supplies. Medicare Advantage Plans must cover all Medicare-covered OUD services but may have specific network requirements and copayments.
- Medicaid: Medicaid also provides comprehensive coverage for substance use disorder treatment, including opioid rehab. If you have both Medicare and Medicaid, you typically pay nothing for services through your state Medicaid program.
We strongly encourage you to verify your insurance coverage with us. We can help you understand your benefits and explore financial assistance options if needed. Don’t forget to check for free Rehab Resources in your area, as non-profit and state-funded programs can offer valuable support. To get started, verify your insurance now.
How to Support a Loved One Through Recovery
Witnessing a loved one struggle with OUD is incredibly painful, and knowing how to help can be confusing. Your support is invaluable during their journey through opioid rehab and into long-term recovery.
- Reduce Stigma: Addiction is a medical condition, not a moral failing. By treating it as such, you help create a safe space for your loved one to seek and accept help. The CDC emphasizes that reducing stigma is important to helping loved ones feel safer and healthier.
- Involve Family: Family involvement in treatment, when appropriate, can be very beneficial. Therapy can help improve communication and heal relationships, fostering a more supportive home environment.
- Encourage Treatment, Not Enabling: While it’s important to be supportive, it’s equally crucial to avoid enabling behaviors that perpetuate substance use. Setting healthy boundaries is an act of love.
- Educate Yourself: Learn about OUD, treatment options, and the recovery process. The more you understand, the better equipped you’ll be to offer meaningful support.
- Carry Naloxone: As discussed earlier, carrying Naloxone can be a lifesaving measure if your loved one experiences an overdose.
- Seek Your Own Support: Supporting someone in recovery can be emotionally taxing. Consider joining support groups for family members of individuals with addiction.
Your role in their recovery journey is significant. For inspiration and hope, read some Addiction Success Stories. We also offer resources to guide you: download our family support guide and learn about family involvement in recovery.
Frequently Asked Questions about Opioid Treatment
We understand that you likely have many questions as you consider opioid rehab. Here, we address some of the most common inquiries to provide clarity and peace of mind.
How long does opioid rehab take?
The duration of opioid rehab is highly individualized and depends on various factors, including the severity of the OUD, the presence of co-occurring mental health conditions, and personal progress. However, research offers clear guidance:
- Typical Program Lengths: Many inpatient and residential treatment facilities offer programs lasting 30, 60, or 90 days. Outpatient programs can also vary in length, with some lasting three months or more.
- Optimal Outcomes: Studies consistently show that individuals who remain in treatment for at least 90 days experience the best long-term outcomes. This duration allows enough time to break old habits, develop new coping skills, and solidify a foundation for sustained sobriety.
- Factors Influencing Duration: Your treatment team will assess your needs and recommend a program length. Flexibility is key, as some individuals may benefit from longer stays or a step-down approach through different levels of care.
We offer various program lengths to accommodate diverse needs, including options like 28 Day Rehabs Near Me for initial stabilization. To get a better understanding of what your journey might look like, you can learn more about what to expect in rehab. For a personalized discussion about program lengths that might suit your situation, please speak to our team about program lengths.
What is the difference between inpatient and outpatient rehab?
Understanding the distinction between inpatient and outpatient opioid rehab is crucial for choosing the most appropriate level of care.
- Inpatient Drug Rehab: This option involves living at the treatment facility 24 hours a day, 7 days a week. It provides a highly structured, immersive environment free from external triggers and distractions. Inpatient programs offer intensive therapy, medical supervision, and a strong sense of community support. It’s ideal for individuals with severe OUD, those with co-occurring mental health disorders, or those who need a complete change of environment to focus on recovery. You can compare Inpatient Drug Rehab options.
- Outpatient Programs: This approach allows individuals to continue living at home while attending scheduled treatment sessions at a facility. Outpatient programs offer more flexibility, enabling clients to maintain work, school, or family responsibilities. They are suitable for individuals with milder OUD, strong support systems at home, or those transitioning from an inpatient program. Outpatient options include Partial Hospitalization Programs (PHPs) and Intensive Outpatient Programs (IOPs). You can explore our Outpatient Programs in more detail.
The choice between inpatient and outpatient care is a significant one that should be made in consultation with addiction professionals. We can help guide you through this decision, ensuring you choose the right path for your unique needs. Learn more about choosing the right program or simply get help choosing your program by contacting us today.
Is treatment for opioid addiction confidential?
Absolutely. Confidentiality is a cornerstone of ethical and effective opioid rehab and addiction treatment. We understand the sensitive nature of seeking help for OUD, and protecting your privacy is our utmost priority.
All reputable treatment providers, including SoberSteps, adhere to strict federal and state regulations regarding patient confidentiality, most notably the Health Insurance Portability and Accountability Act (HIPAA) and federal regulations governing substance use disorder patient records (42 CFR Part 2). These laws ensure that your personal health information, including your participation in treatment, is protected and cannot be shared without your explicit consent, except in very limited circumstances mandated by law (e.g., medical emergencies, court orders).
At SoberSteps, we cultivate an environment of trust and discretion. You can seek Confidential Mental Health Support without fear of your information being disclosed. Our team is trained to handle your inquiries and treatment details with the highest level of privacy and respect. If you have any concerns or questions about confidentiality, we encourage you to speak with a confidential advisor now. We are transparent about our practices; you can also learn about our privacy policy.
Conclusion: Your Journey to a Sober Life Starts Now
Recovery is a journey, not a destination. It’s a continuous process of growth, learning, and resilience. Opioid addiction is a treatable disease—a chronic condition that can be managed effectively with the right support and resources. Hope and healing are not just possibilities; they are within reach for you or your loved one.
At SoberSteps, we believe in the power of comprehensive, compassionate care. We’ve seen countless individuals transform their lives through dedicated opioid rehab programs that combine medical expertise with therapeutic support. Our mission is to connect you with the best possible treatment options, guiding you through every step, from initial assessment to long-term aftercare.
If you’re ready to take the first step towards a healthier, sober life, or if you’re seeking help for a loved one, we are here for you. SoberSteps provides a confidential 24/7 helpline, ready to connect you with treatment options that fit your unique needs. Don’t let fear or uncertainty hold you back from the life you deserve.
Find the best drug rehab for you or Contact Us today to take the first step. We are committed to empowering you through your recovery journey. Read more about our mission and how we help. Your journey to a sober life starts now. Start your recovery today.



