Understanding Alcohol Withdrawal: What You Need to Know
Alcohol Withdrawal: Symptoms, Treatment & Timeline is a critical topic for anyone struggling with alcohol dependence or supporting someone who is. When your body becomes physically dependent on alcohol, stopping or reducing your intake triggers a syndrome that ranges from uncomfortable to life-threatening. Here’s what you need to know right away:
Quick Overview:
- Symptoms begin 6-24 hours after the last drink and include tremors, anxiety, nausea, sweating, and in severe cases, seizures and delirium tremens (DTs)
- Timeline typically peaks at 48-72 hours, with most physical symptoms resolving within 7-10 days, though some psychological symptoms can last months
- Treatment requires medical supervision, often including benzodiazepines, 24/7 monitoring, and nutritional support to prevent life-threatening complications
- Danger lies in severe complications like seizures and DTs, which can be fatal without proper medical care
More than 29 million Americans struggled with alcohol use disorder in 2022, and approximately 50% of those who are physically dependent will experience withdrawal symptoms when they stop drinking. The severity varies widely. Some people experience mild anxiety and tremors. Others face medical emergencies requiring intensive care.
Your brain adapts to alcohol’s constant presence by changing how it produces certain chemicals. When you suddenly stop drinking, your central nervous system goes into overdrive. This creates the dangerous symptoms of withdrawal. The mortality rate for severe alcohol withdrawal can be as high as 20% without treatment, but drops to less than 5% with proper medical care.
This is why attempting to “quit cold turkey” alone is extremely risky. Professional detox provides the safety net you need.
At Sober Steps, we’ve dedicated our work to helping individuals steer the complexities of recovery, including understanding Alcohol Withdrawal: Symptoms, Treatment & Timeline and connecting people with confidential, life-saving treatment resources. Our mission is ensuring no one faces these challenges alone, and we’re available 24/7 at (844) 491-5566 to provide immediate, anonymous support.
Alcohol Withdrawal: Symptoms, Treatment & Timeline
Understanding the nuances of Alcohol Withdrawal: Symptoms, Treatment & Timeline is essential for anyone seeking or providing support on the path to recovery. This section defines the core aspects of alcohol withdrawal, providing a comprehensive overview for those seeking to understand the process. For immediate, confidential guidance, call our 24/7 helpline at (844) 491-5566.
What Causes Alcohol Withdrawal?
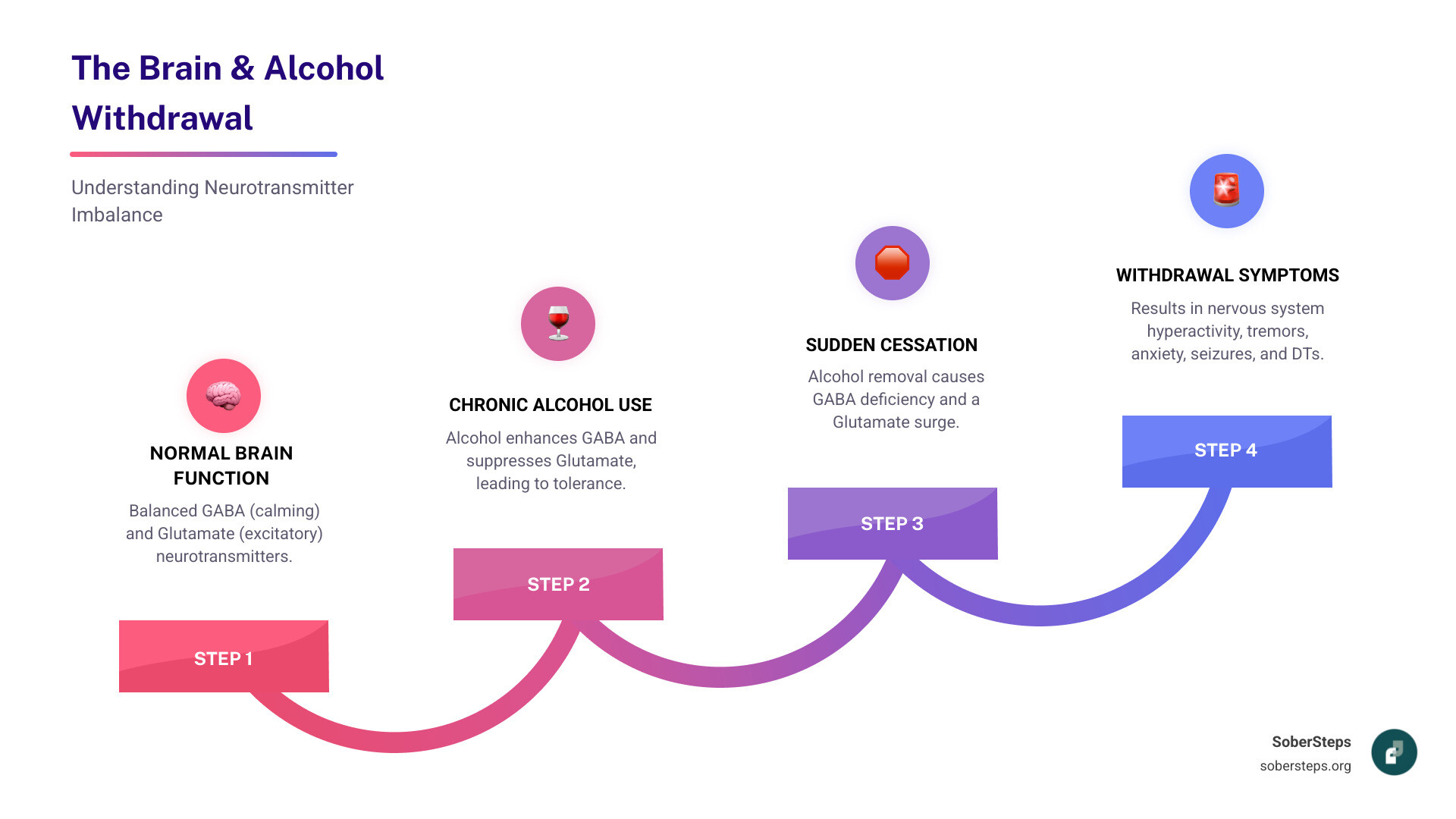
Alcohol withdrawal syndrome (AWS) occurs when someone who is physically dependent on alcohol suddenly stops drinking or significantly reduces their intake. To fully grasp why withdrawal happens, we need to look at what alcohol does to the brain.
Alcohol is a central nervous system (CNS) depressant. This means it slows down brain activity. When someone drinks heavily and consistently over time, their brain adapts to this constant presence of alcohol. It tries to counteract the depressant effects by increasing the activity of excitatory neurotransmitters like glutamate and decreasing the activity of inhibitory neurotransmitters like Gamma-aminobutyric acid (GABA). This creates a new, altered chemical balance.
The problem arises when alcohol is suddenly removed from the system. The brain, still in its hyper-alert, overexcited state, can no longer regulate itself fast enough. The balance of neurotransmitters is thrown off: there’s too much glutamate (excitatory) and not enough GABA (inhibitory). This neurotransmitter imbalance leads to brain hyperactivity, causing the wide range of symptoms we associate with alcohol withdrawal. It’s like an accelerating vehicle that suddenly loses its brakes.
For more in-depth information on the scientific research behind alcohol’s effects on the brain, you can refer to Scientific research on alcohol’s effect on the brain.
A Closer Look at Alcohol Withdrawal Symptoms
The symptoms of alcohol withdrawal can vary significantly from person to person, depending on factors like the severity and duration of alcohol use, overall health, and genetic predisposition. However, many common physical and psychological symptoms emerge.
Common symptoms of alcohol withdrawal include:
- Physical symptoms:
- Tremors (often called “the shakes”)
- Nausea and vomiting
- Headache
- Excessive sweating
- Increased heart rate (tachycardia)
- High blood pressure
- Dilated pupils
- Rapid breathing
- Loss of appetite
- Hyperthermia (liftd body temperature)
- Psychological symptoms:
- Anxiety
- Insomnia and other sleep problems (difficulty falling or staying asleep, vivid dreams)
- Irritability and agitation
- Hypervigilance
- Confusion
- Mood swings
- Hallucinations (auditory, visual, or tactile)
- Paranoia
While some symptoms, like mild anxiety and tremors, might be uncomfortable but not life-threatening, others, such as severe hallucinations and seizures, can be extremely dangerous. These symptoms are not just “in your head”; they are real physiological responses to your body adjusting to the absence of alcohol.
Navigating the Alcohol Withdrawal Treatment & Timeline
Successfully navigating alcohol withdrawal involves understanding its typical progression, the variability in its duration, and the factors that influence an individual’s experience. This journey is commonly broken down into stages, each with its own set of expected symptoms and risks.
Stages of Withdrawal: Alcohol withdrawal symptoms typically begin within six to 24 hours of stopping or significantly decreasing heavy, long-term alcohol use. The intensity often peaks around 48-72 hours. While physical symptoms usually resolve within seven to 10 days, some psychological symptoms, often referred to as Post-Acute Withdrawal Syndrome (PAWS), can persist for several months.
Duration Variability: Everyone’s detox and withdrawal timeline is different. A survey of 2,136 American adults found that withdrawal symptoms lasted an average of 4.83 days, with 95% of respondents reporting symptoms lasting two to eight days. However, for some, symptoms may linger for weeks.
Factors Influencing Timeline and Severity: Several factors can influence how long withdrawal lasts and how severe it becomes:
- Age: Older individuals, especially those over 65, may be at higher risk for severe withdrawal.
- Gender: While not a direct predictor, physiological differences can impact how the body processes alcohol.
- Health Status: Co-occurring physical or mental health conditions, dehydration, electrolyte imbalances, and abnormal liver function can all exacerbate withdrawal symptoms.
- History of Alcohol Use: The frequency, length, and amount of alcohol consumed are significant predictors. Heavy daily alcohol users are more likely to experience severe symptoms, including hallucinations, delirium tremens, and seizures.
- Previous Withdrawal Episodes: A phenomenon called “kindling” suggests that each subsequent withdrawal episode tends to be more severe than the last. This means previous experiences with withdrawal increase the risk of more dangerous symptoms.
The Clinical Institute Withdrawal Assessment for Alcohol, Revised (CIWA-Ar) scale is a common tool used by medical professionals to assess the severity of AWS. Scores of 8 or less typically indicate mild withdrawal, 8-15 suggest moderate withdrawal, and scores above 15 imply severe withdrawal and a higher risk for major complications.
The Alcohol Withdrawal Timeline: A Stage-by-Stage Guide
This timeline provides a general guide to what you might expect during alcohol withdrawal, but individual experiences can vary greatly. Attempting to manage this process alone can be dangerous, potentially leading to severe, life-threatening complications. Call (844) 491-5566 to speak with a specialist about safe detox options.
Stage 1: 6-12 Hours After Last Drink
This is often when the first, milder symptoms of alcohol withdrawal begin to appear. These initial symptoms can be uncomfortable but are usually not life-threatening on their own.
- Anxiety: A feeling of nervousness or unease.
- Insomnia: Difficulty falling or staying asleep.
- Headache: Ranging from mild to severe.
- Stomach upset: Nausea, vomiting, or loss of appetite.
- Heart palpitations: A feeling of a rapid, fluttering, or pounding heart.
- Tremors: Shaking, particularly in the hands.
These symptoms typically start about 6-12 hours after your last drink, as the alcohol levels in your bloodstream begin to drop. While they might feel like an intense hangover, they are the initial signs that your body is reacting to the absence of alcohol. For more information on early withdrawal symptoms, you can consult Information on early withdrawal symptoms.
Stage 2: 12-48 Hours After Last Drink
As withdrawal progresses, symptoms can intensify and become more concerning. This stage is particularly critical due to the increased risk of severe complications.
- Intensified Symptoms: The symptoms from Stage 1 often become more pronounced.
- Hallucinations: Some individuals may experience visual, auditory, or tactile hallucinations. These can range from seeing patterns or shadows to hearing voices or feeling things crawling on their skin. Alcohol hallucinosis usually begins within 12 to 24 hours after the last drink and can last up to two days.
- Withdrawal Seizures: The risk of seizures is highest during this period, typically occurring between 6 to 48 hours after the last drink, with the risk peaking around 24 hours. These can be generalized tonic-clonic seizures (grand mal seizures) and are a medical emergency.
- Increased Blood Pressure and Heart Rate: Your vital signs may become significantly liftd as your central nervous system goes into overdrive.
- Body Temperature Increase: You might develop a mild fever or hyperthermia.
Stage 3: 48-72 Hours After Last Drink

This period often represents the peak severity of alcohol withdrawal symptoms. It’s when the most dangerous complications, including Delirium Tremens (DTs), are most likely to occur.
- Peak Symptom Severity: All previous symptoms may reach their most intense levels.
- Delirium Tremens (DTs) Risk Highest: DTs typically appear from 48 to 72 hours after the last drink. This is a severe and potentially fatal form of withdrawal that requires immediate medical intervention.
- Severe Confusion and Disorientation: You may struggle to understand where you are, who you are, or what is happening around you.
- Agitation: Extreme restlessness and emotional distress.
- Fever: High body temperature.
- Tachycardia: A dangerously fast heart rate.
While many physical symptoms begin to subside after 72 hours, some individuals may continue to experience psychological symptoms, sometimes for weeks or even months. This extended period of psychological discomfort is known as Post-Acute Withdrawal Syndrome (PAWS).
Dangers and Complications of Alcohol Withdrawal
It is critical to recognize the potential dangers of alcohol withdrawal. Severe symptoms require immediate medical intervention. If you or a loved one is at risk, call (844) 491-5566 now.
What is Delirium Tremens (DTs)?
Delirium Tremens (DTs) is the most severe and potentially life-threatening manifestation of alcohol withdrawal. It is a medical emergency that occurs in about 3% to 5% of people with alcohol use disorder who are going through withdrawal, particularly in individuals with a long history of heavy alcohol use.
DTs are characterized by:
- Delirium: A state of severe confusion, disorientation, and reduced awareness of the environment.
- Severe Agitation: Extreme restlessness, anxiety, and sometimes aggressive behavior.
- Disorientation: Inability to recognize time, place, or people.
- Autonomic Hyperactivity: Dangerous fluctuations in vital signs, including high fever, rapid heart rate (tachycardia), and dangerously high blood pressure.
- Profound Hallucinations: Often vivid and disturbing, leading to extreme fear or paranoia.
Historically, the mortality rate for DTs was as high as 20% without treatment. However, with advances in critical care and prompt medical intervention, this rate has significantly decreased. According to the U.S. medical resource Medscape, the mortality rate with treatment is now less than 5%. Despite this improvement, DTs remain a serious condition that necessitates immediate professional medical care.
Risk Factors for Severe Withdrawal
While predicting the exact course of alcohol withdrawal can be challenging, certain factors significantly increase the risk of experiencing severe symptoms, including seizures and Delirium Tremens:
- History of Heavy, Long-Term Drinking: The longer and heavier the alcohol use, the more dependent the brain becomes, and the more severe the withdrawal is likely to be. The risk of experiencing severe symptoms like delirium tremens and seizures is significantly higher for those with a history of heavy, daily alcohol use.
- Previous Withdrawal Episodes: The “kindling effect” means that each time a person goes through withdrawal, the subsequent episodes tend to be more severe, making them more susceptible to complications.
- Co-occurring Medical Conditions: Conditions like liver disease, heart problems, infections, or head injuries can complicate withdrawal and increase its severity.
- Older Age: Individuals over 65 may have a higher risk of severe withdrawal due to reduced physiological reserves and potential co-morbidities.
- Poor Nutrition: Chronic alcohol abuse often leads to nutritional deficiencies (e.g., thiamine, magnesium), which can worsen withdrawal symptoms and increase the risk of complications like Wernicke’s encephalopathy.
- History of Withdrawal Seizures: Having experienced seizures during previous withdrawal episodes is a strong predictor for future seizures and progression to DTs.
When to Seek Professional Help
Given the potential dangers of alcohol withdrawal, it is almost always recommended to seek professional medical help. Attempting to detox at home without medical supervision is incredibly risky and can be fatal.
You should seek immediate professional help if you or someone you know experiences any of the following emergency signs during alcohol withdrawal:
- Seizures
- Hallucinations (seeing, hearing, or feeling things that aren’t there)
- Severe confusion or disorientation
- High fever
- Chest pain
- Irregular or very rapid heartbeat
- Inability to stop drinking despite trying
- Extreme agitation or paranoia
- Any symptoms that worsen or become unmanageable
Even if symptoms seem mild, consulting a healthcare professional is wise. They can assess your risk level, monitor your condition, and provide a safe and comfortable detoxification process. Detoxing alone is not recommended. If you are experiencing concerning symptoms, call (844) 491-5566 for immediate guidance.
Professional Treatment for Alcohol Withdrawal
Professional treatment provides a safe, medically supervised environment to manage withdrawal symptoms and begin the journey to recovery. This approach ensures not only your physical safety but also sets the foundation for long-term sobriety.
The Role of Medical Detoxification
Medical detoxification is often the first and most critical step in treating alcohol use disorder. It involves a structured program designed to safely manage the physical symptoms of alcohol withdrawal under the care of medical professionals. The goal of alcohol detox is to help you reach an alcohol-free state, relieve your symptoms, and address any co-occurring conditions, preparing you for further addiction treatment.
Key aspects of medical detox include:
- 24/7 Medical Supervision: Medical staff are present around the clock to monitor vital signs, assess symptoms, and intervene if complications arise. This constant oversight is crucial for preventing life-threatening events like seizures or DTs.
- Symptom Management: Medications are administered to alleviate the discomfort of withdrawal symptoms.
- Safety and Comfort: Detox centers strive to create a quiet, low-lit, and minimally stimulating environment to help keep you calm and reduce distress.
- Prevention of Severe Complications: Early detection and appropriate treatment during detox can reduce the mortality rate for severe AWS from as high as 20% without treatment to less than 5% with treatment.
- Inpatient vs. Outpatient Detox: The choice depends on the severity of dependence, medical history, and risk factors. Inpatient detox offers the highest level of supervision and is recommended for those at high risk of severe withdrawal. Outpatient options may be suitable for individuals with milder symptoms and strong social support.
- Nutritional Support: Chronic alcohol use often leads to nutritional deficiencies. Detox programs address this with proper nutrition, hydration, and often vitamin supplements (like thiamine, folate, and magnesium) to correct imbalances and prevent conditions like Wernicke’s encephalopathy.
Alcohol detox programs typically last 3-7 days, but this can vary based on individual needs and symptom severity.
Medications Used in Alcohol Withdrawal Treatment
Medication plays a vital role in making alcohol withdrawal safer and more tolerable. These medications primarily work to calm the overactive central nervous system and prevent severe complications.
- Benzodiazepines (First-Line Treatment): These are the most commonly used and effective medications for managing AWS. They work by enhancing the effects of GABA, helping to restore the brain’s chemical balance and reduce hyperexcitability. Examples include:
- Lorazepam: Often preferred for individuals with liver impairment or older patients due to its shorter half-life.
- Diazepam: Known for its rapid onset and long duration of action, making it effective for sustained symptom control.
Benzodiazepines can reduce the incidence of seizures by up to 84% and prevent the development of DTs within the first 2 days of withdrawal.
- Anticonvulsants: Medications like carbamazepine or gabapentin may be used as adjuncts or alternatives to benzodiazepines, particularly for managing withdrawal seizures.
- Beta-blockers: Drugs like atenolol or propranolol can help manage autonomic symptoms such as rapid heart rate and high blood pressure, though they don’t prevent seizures or DTs.
- Clonidine: An alpha-2 agonist, it can also help reduce some autonomic symptoms like sweating and tremors but is not a substitute for benzodiazepines in preventing severe withdrawal.
Medications are typically administered using either symptom-triggered regimens (dosed based on the severity of current symptoms, often guided by scales like CIWA-Ar) or fixed-dose regimens (a scheduled, tapering dose over several days). Symptom-triggered regimens often lead to lower total medication doses and shorter treatment durations without compromising safety.
Long-Term Support and Recovery
While medical detox is a crucial first step, it is not a cure for alcohol use disorder. It addresses the immediate physical dangers of withdrawal. The journey to lasting sobriety requires ongoing support and comprehensive treatment strategies.
- Detox is the First Step: After safely completing detox, the focus shifts to addressing the underlying causes of alcohol dependence and developing coping mechanisms for a sober life.
- Therapy and Counseling: Various forms of therapy are essential for long-term recovery.
- Cognitive-Behavioral Therapy (CBT): Helps individuals identify and change negative thought patterns and behaviors related to alcohol use.
- Family Therapy: Involves family members in the recovery process, addressing dynamics that may contribute to addiction.
- Mutual-Help Groups: Participation in groups provides peer support, shared experiences, and a sense of community.
- Building a Sober Life: This involves developing new healthy routines, hobbies, and support networks. It also includes learning strategies to manage cravings and prevent relapse, especially if experiencing Post-Acute Withdrawal Syndrome (PAWS), where psychological symptoms like mood swings, anxiety, and low energy can persist for months. PAWS can cause relapse, so being prepared and having coping skills is vital.
The long-term outlook for alcohol addiction treatment depends heavily on continued engagement in recovery efforts. Patients may still experience sleep disturbances, mood swings, and low energy levels in the months after treatment. However, with consistent support and dedication, complete recovery and a fulfilling, sober life are absolutely possible. For confidential information on long-term treatment options, call (844) 491-5566.
Frequently Asked Questions about Alcohol Withdrawal
Can alcohol withdrawal be fatal?
Yes, alcohol withdrawal can be fatal. Severe complications like Delirium Tremens (DTs) and seizures pose significant risks to life. Without proper medical intervention, DTs can lead to heart failure, respiratory arrest, or other severe medical emergencies. Medically supervised detox significantly reduces this risk by providing monitoring and medication to prevent these dangerous complications.
How long does alcohol withdrawal last?
The duration of alcohol withdrawal varies for each individual. Physical symptoms typically begin within 6-12 hours after the last drink, peak around 48-72 hours, and usually subside within seven to 10 days. However, some psychological symptoms, known as Post-Acute Withdrawal Syndrome (PAWS), such as anxiety, depression, and sleep disturbances, can persist for weeks or even months after the acute physical withdrawal has ended.
Is it safe to detox from alcohol at home?
Detoxing from alcohol at home without medical supervision is not recommended and can be extremely dangerous. The risk of severe complications like seizures, Delirium Tremens (DTs), and other medical emergencies is too high. These complications can appear suddenly and be life-threatening. Professional medical detox provides the necessary oversight, medication, and support to ensure a safe and comfortable withdrawal process.
Begin Your Recovery Journey Safely
Understanding the Alcohol Withdrawal: Symptoms, Treatment & Timeline is the first step, but taking action is what saves lives. Withdrawal is a serious medical condition that requires professional care for a safe and successful outcome. You don’t have to face this alone. SoberSteps provides a confidential and anonymous platform to connect you with the help you need. Your path to a healthier, sober life can start today. Call our 24/7 helpline at (844) 491-5566 for immediate, private support.



