
The Dual Nature of Ketamine: From Operating Room to Treatment Room
Ketamine addiction therapy represents one of the most complex and evolving areas in addiction medicine today. If you’re searching for information about ketamine as a treatment tool, here’s what you need to know:
Quick Answer: Ketamine Addiction Therapy Overview
- What it is: A supervised medical treatment using controlled ketamine doses alongside psychotherapy to address substance use disorders
- How it works: By promoting neuroplasticity and creating a “therapeutic window” where psychological interventions become more effective
- Primary uses: Treatment-resistant depression, alcohol use disorder, cocaine addiction, and opioid use disorder
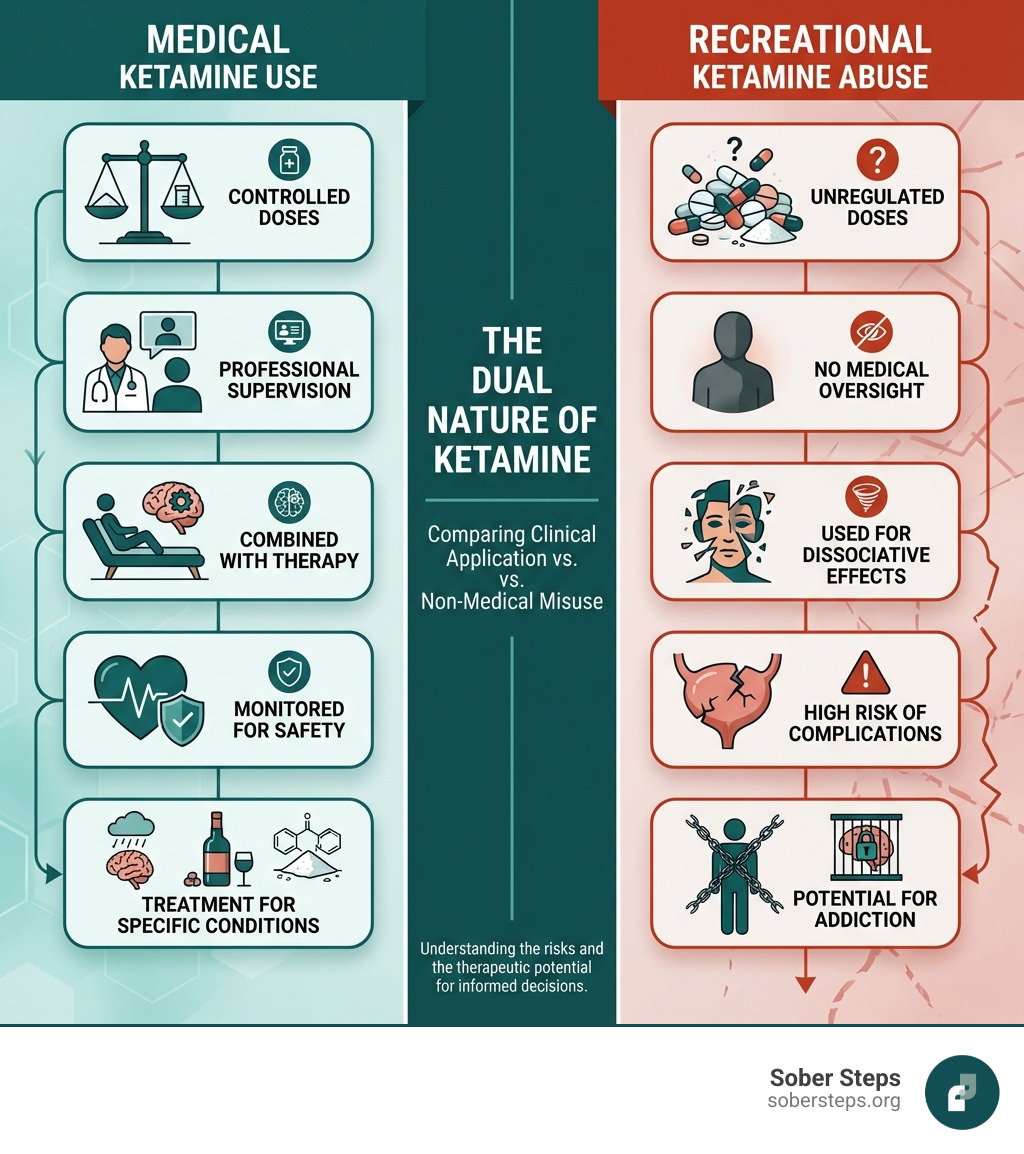
- Key difference: Medical ketamine is precisely dosed and administered by professionals; recreational ketamine is unregulated and dangerous
- Success factors: Must be combined with behavioral therapy; requires ongoing medical supervision
- Risks to know: Ketamine itself has addiction potential; only effective in controlled clinical settings
Ketamine occupies a unique and somewhat paradoxical place in modern medicine. Originally developed in the 1960s as an anesthetic, it became a staple in operating rooms and emergency medicine for its safety profile and rapid action. But ketamine also gained notoriety as a recreational drug—known on the streets as “Special K”—used for its dissociative and hallucinogenic effects.
Now, ketamine is experiencing a third chapter in its story: as a potential breakthrough treatment for mental health conditions and addiction itself. In 2019, the FDA approved esketamine (a ketamine derivative) for treatment-resistant depression, marking a significant shift in how we view this drug. Recent research suggests ketamine, when combined with psychological therapy, may help people struggling with alcohol, cocaine, and opioid addiction maintain abstinence and reduce cravings.
This dual nature—both a potential treatment and a substance of abuse—makes ketamine uniquely challenging to understand. The same properties that make it effective in a clinical setting can lead to psychological dependence when misused recreationally. According to research, self-reported nonmedical use of ketamine reached 0.9% in the United States in 2019, while the number of adults requiring treatment for ketamine use disorder has risen fivefold since 2015.
The key distinction lies in how ketamine is used. In supervised medical settings, low doses are carefully administered alongside evidence-based psychotherapy. In recreational contexts, users often take much higher, uncontrolled doses without therapeutic support—a practice that can lead to serious physical complications including bladder damage, cognitive impairment, and addiction itself.
At Sober Steps, we understand the complexities of navigating ketamine addiction therapy and help individuals find trustworthy, evidence-based treatment programs. Our mission is to connect those struggling with addiction to the comprehensive resources they need for lasting recovery.
Understanding Ketamine: How It Works and Why It’s Different
To truly understand how ketamine addiction therapy works, we first need to dig into the fascinating mechanics of ketamine itself. Ketamine is classified as a dissociative anesthetic, meaning it can create a sense of detachment from one’s body and surroundings. Its primary action in the brain is through its role as a noncompetitive antagonist of the N-methyl-D-aspartate (NMDA) receptor.
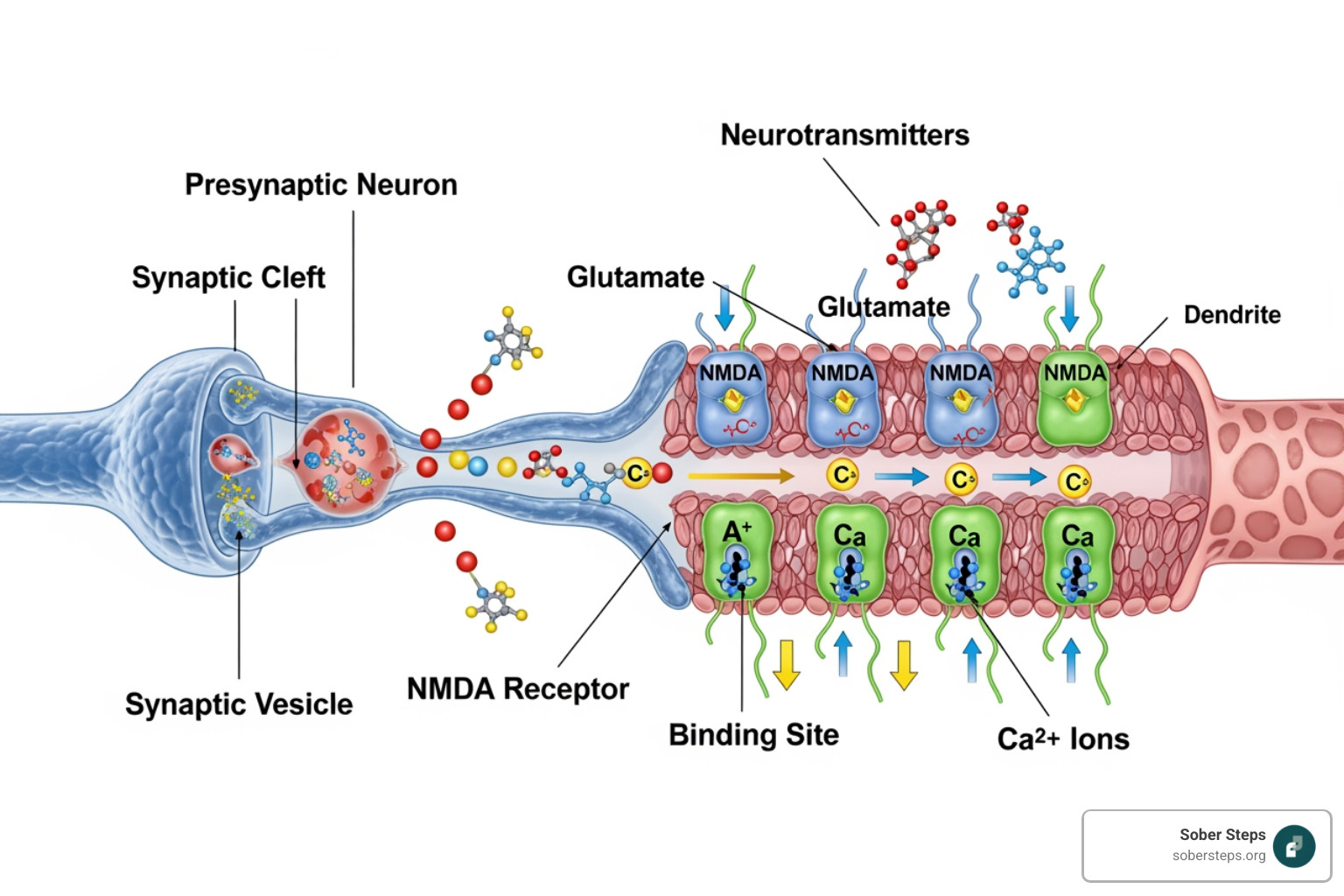
Think of your brain as a busy city with countless roads and intersections—these are your neural pathways and synapses. Neurotransmitters are the vehicles that carry messages across these intersections. One crucial neurotransmitter is glutamate, which excites brain cells and plays a vital role in learning and memory. Ketamine essentially modulates the glutamate system by temporarily blocking the NMDA receptors, which are a type of glutamate receptor. This blocking action can lead to a cascade of beneficial effects.
One of the most exciting aspects of ketamine’s mechanism is its ability to promote neuroplasticity. This refers to the brain’s capacity to reorganize itself by forming new neural connections and strengthening existing ones. Ketamine triggers increased activity of glutamate in the frontal cortex, which in turn promotes the formation of new synapses. This process, known as synaptogenesis, is believed to be crucial for its rapid antidepressant effects and its potential in addiction treatment. Markers like Brain-Derived Neurotrophic Factor (BDNF), a protein that supports the survival of existing neurons and encourages the growth and differentiation of new neurons and synapses, are often associated with these changes.
Beyond its direct neurochemical effects, ketamine also possesses unique dissociative and psychedelic properties. At lower doses, it can induce mild visual hallucinations and a sense of heightened awareness. At higher, recreational doses, it can lead to vivid hallucinations, an “out-of-body” experience, and temporary memory loss. These effects, while potentially dangerous in recreational settings, are carefully managed in therapeutic contexts to facilitate a “therapeutic window” where individuals may gain new perspectives on their thoughts and behaviors. The rapid-acting nature of ketamine means its effects on consciousness can be relatively brief, typically lasting a few hours, yet the neuroplastic changes it initiates can have more sustained impacts.
For a deeper dive into the scientific understanding of ketamine’s mechanisms, you can refer to scientific research on ketamine’s mechanisms.
Therapeutic Uses for Depression and Addiction
Initially used as an anesthetic, ketamine has found new life in the medical community for its profound impact on mental health. One of its most significant breakthroughs is in the treatment of severe, treatment-resistant depression and suicidal ideation. For individuals who have not responded to traditional antidepressant medications, ketamine, or its derivative esketamine (brand name Spravato), has offered a guide of hope. Esketamine, an S-enantiomer of ketamine, received FDA approval for depression in 2019 for those with treatment-resistant depression and suicidal thoughts. This nasal spray requires careful administration and supervision by a medical expert, highlighting the importance of a controlled clinical setting.
Beyond depression, researchers are actively exploring ketamine’s potential in ketamine addiction therapy for various substance use disorders:
- Alcohol Use Disorder (AUD): Studies have shown that ketamine, when combined with psychological therapy, can effectively prolong abstinence from alcohol in detoxified individuals. One clinical trial demonstrated that participants receiving ketamine alongside therapy had better outcomes than those receiving therapy alone. Ketamine may help by “rewriting drinking memories” and alleviating depressive symptoms, which are common triggers for relapse in AUD.
- Cocaine Addiction: Similar promising results have been observed for cocaine addiction. Research indicates that ketamine can reduce craving for and self-administration of cocaine. A study combining a single ketamine infusion with mindfulness-based behavioral modification showed significant improvements in individuals with cocaine dependence.
- Opioid Use Disorder (OUD): Preliminary evidence suggests ketamine may be helpful in treating OUD, particularly as an adjunct to psychotherapy. It has shown potential in reducing opioid cravings and may even facilitate buprenorphine initiation during opioid withdrawal.
The underlying theory for its effectiveness in addiction is that ketamine’s neuroplastic effects can create a “therapeutic window.” During this time, the brain may be more receptive to new learning and behavioral changes, making psychological interventions more potent. This means that combining ketamine with therapies like Cognitive Behavioral Therapy (CBT), Motivational Improvement Therapy, or relapse prevention strategies can improve their effectiveness, helping individuals build new coping mechanisms and thought patterns.
Risks, Side Effects, and Addiction Potential
While the therapeutic potential of ketamine is exciting, it’s crucial to acknowledge its risks, side effects, and potential for addiction, especially when not administered under strict medical supervision.
Ketamine dependence is primarily psychological, meaning individuals develop intense cravings for the drug and a strong desire to re-experience its effects. Unlike some other substances with severe physical withdrawal symptoms, ketamine withdrawal mainly manifests as psychological discomfort, including strong cravings, mood swings, anxiety, depression, insomnia, and irritability. However, physical symptoms like nausea, shakes, sweating, and heart palpitations can also occur. Tolerance to ketamine can develop very rapidly, particularly with binge use, leading users to take increasingly higher doses to achieve the desired effects. High-dose recreational use can also lead to a “K-hole,” an intense dissociative state where users feel completely detached from reality.
Long-term and recreational misuse of ketamine can lead to serious physical health consequences:
- Bladder Damage (Cystitis): One of the most debilitating side effects is ketamine-induced cystitis, a severe inflammation of the bladder that can cause intense pain, urinary frequency, and, in extreme cases, permanent bladder damage requiring surgical intervention. Research indicates that 60% of individuals reporting problematic ketamine use experience bladder problems.
- Cognitive Impairment: Chronic ketamine use can harm the brain, leading to significant cognitive impairments, particularly affecting memory and attention span. Studies on chronic ketamine users have profiled these deficits.
- Cardiovascular Risks: Ketamine can lift blood pressure and heart rate. While generally safe in controlled medical settings, recreational use, especially in individuals with pre-existing heart conditions, can lead to serious cardiovascular complications and, as tragically seen in high-profile cases, acute effects can be fatal.
The nonmedical use of ketamine remains a concern. In 2019, self-reported past-year nonmedical use of ketamine in the United States reached a peak prevalence of 0.9%. The DEA provides further information on ketamine’s risks and its potential for abuse and diversion, particularly when obtained outside of legal medical channels. The tragic death of actor Matthew Perry, attributed to the “acute effects of ketamine,” serves as a stark reminder of the dangers of unsupervised or excessive use.
It’s vital to differentiate between medically supervised ketamine addiction therapy and recreational abuse. In a clinical setting, doses are carefully controlled, and patients are monitored for adverse reactions. Recreational use, however, involves unknown purity, uncontrolled doses, and often polysubstance use, dramatically increasing the risks.
For more information on the risks associated with ketamine, you can consult DEA information on ketamine risks.
Navigating Ketamine Addiction Therapy: What to Expect
If you or a loved one are considering ketamine addiction therapy, understanding what to expect is crucial. This is not a casual endeavor; it’s a specialized medical treatment conducted within a highly structured and supervised environment.

The first step in any reputable program will involve a comprehensive assessment. This isn’t just about your ketamine use; it’s about understanding your overall physical and mental health. Many individuals with substance use disorders also struggle with co-occurring mental health conditions like depression, anxiety, or trauma—a phenomenon known as dual diagnosis. Effective treatment programs integrate psychiatric care to address these conditions alongside therapies focused on changing substance use patterns. This holistic approach ensures that all contributing factors to addiction are identified and addressed.
The importance of a supervised medical setting cannot be overstated. Ketamine administration, even at sub-anesthetic doses, requires professional oversight to monitor vital signs, manage any potential side effects (like transient increases in blood pressure or heart rate), and ensure a safe and therapeutic experience. Reputable clinics adhere to stringent safety guidelines, and medical professionals are trained to handle any emergencies, however rare.
At Sober Steps, we emphasize connecting individuals to programs that prioritize these safety measures and offer comprehensive, evidence-based care. For more details on the types of comprehensive programs available, you can explore more info about treatment programs.
Detoxification and Managing Withdrawal
The journey through ketamine addiction therapy often begins with detoxification, the process of safely ridding the body of the drug. While ketamine withdrawal is primarily psychological, it can be uncomfortable and challenging.
Common ketamine withdrawal symptoms include:
- Intense cravings for the drug
- Low mood and depression
- Anxiety and irritability
- Insomnia and other sleep disturbances
- Fatigue
- Nausea and stomach pain (“K-cramps”)
- Shaking and sweating
- Heart palpitations
Because ketamine withdrawal can involve significant psychological distress, including potential psychotic symptoms in some cases, medical supervision during detox is highly recommended. This ensures that any symptoms are managed safely and effectively, potentially with medications to alleviate discomfort and reduce cravings. Unlike withdrawal from substances like opioids or alcohol, which often have severe and dangerous physical symptoms, the primary challenge with ketamine withdrawal lies in managing the intense psychological urges and mood disturbances. However, this doesn’t make it any less difficult, and professional support is key to preventing relapse during this vulnerable period.
The Core Components of Ketamine Addiction Therapy
Once detoxification is complete, the therapeutic phase of ketamine addiction therapy begins. This approach is rarely about ketamine alone; it’s about integrating the drug’s unique properties with robust psychological support. The goal is to maximize the “therapeutic window” that ketamine can open.
Key components often include:
- Ketamine-Assisted Psychotherapy (KAP): This is a specialized form of therapy where ketamine is administered in a controlled session, followed by integration therapy. The dissociative and psychedelic effects of ketamine can help individuals access deeper insights, process trauma, and gain new perspectives on their addiction patterns. The experience is then processed with a therapist to integrate these insights into lasting behavioral change.
- Individual Therapy: One-on-one sessions with a therapist are crucial for addressing the underlying psychological factors contributing to addiction. This can include Cognitive Behavioral Therapy (CBT), which helps identify and change negative thought patterns, or Motivational Interviewing (MI), which strengthens a person’s motivation for change. Trauma-informed therapies are also vital for those with co-occurring trauma.
- Group Therapy: Sharing experiences with peers who understand the struggle of addiction can be incredibly powerful. Group therapy provides a supportive community, reduces feelings of isolation, and offers different perspectives and coping strategies.
- Relapse Prevention Strategies: A core focus of therapy is to equip individuals with the tools to prevent future relapse. This involves identifying triggers, developing healthy coping mechanisms, and building a strong support network. When combined with ketamine, these strategies may be more effectively learned and integrated due to the brain’s improved neuroplasticity.
The idea is that ketamine doesn’t “cure” addiction on its own. Instead, it creates a unique state of mind where psychotherapy can be more effective. This “therapeutic window” allows for deeper psychological processing and the potential for new neural connections to form, making it easier to break free from old, addictive patterns.
How Ketamine Addiction Therapy Differs from Other Treatments
Ketamine addiction therapy stands apart from many traditional addiction treatments due to its unique neurobiological mechanisms and its potential to rapidly facilitate psychological change. While traditional approaches remain vital, ketamine offers a distinct pathway that can complement or improve existing modalities.
Here’s a comparison to illustrate some key differences:
| Feature | Ketamine Addiction Therapy | Traditional 12-Step Programs | Medication-Assisted Treatment (MAT) for Opioids/Alcohol |
|---|---|---|---|
| Primary Mechanism | Neuroplasticity, NMDA receptor modulation, creation of a “therapeutic window” for improved psychotherapy, disruption of drug memories. | Peer support, spiritual awakening, acceptance, surrender, character defects, making amends, mutual aid. | Opioid receptor modulation (e.g., buprenorphine, naltrexone) or GABAergic system modulation (e.g., acamprosate) to reduce cravings and block euphoric effects. |
| Role of Medication | Ketamine is administered in controlled, therapeutic doses as an adjunct to psychotherapy. | Typically abstinent from all substances; medications may be used for co-occurring mental health, but not as part of the core 12-step philosophy itself. | Medications (e.g., buprenorphine, naltrexone, acamprosate) are a central component, often taken daily for extended periods. |
| Focus of Treatment | Rapidly addresses depressive symptoms, reduces cravings, facilitates psychological breakthroughs, improves receptivity to therapy. | Spiritual and personal growth, accountability, community, addressing character flaws, making amends. | Reduces cravings, prevents withdrawal, blocks euphoric effects of substances, stabilizes brain chemistry. |
| Psychological Potential | Potential for profound personal insights, processing trauma, and “rewriting” maladaptive memories due to dissociative/psychedelic effects. | Encourages self-reflection, confession, and narrative reconstruction within a group setting. | Focuses on reducing physical dependence to allow for engagement in behavioral therapies; does not directly induce altered states of consciousness for therapeutic insight. |
| Treatment Course | Can involve a series of infusions or sessions over weeks/months, potentially offering rapid and sustained effects, especially for depression. | Ongoing, lifelong process of attendance at meetings and working through steps. | Often long-term, continuous medication management, sometimes for years. |
| Addiction Type | Showing promise for Alcohol Use Disorder, Cocaine Use Disorder, and Opioid Use Disorder. | Applicable across a wide range of substance use disorders and behavioral addictions. | Primarily for opioid and alcohol use disorders. |
While ketamine is a medication, it’s not a replacement medication in the same way buprenorphine or methadone are for opioid use disorder. Instead, it serves as an adjunctive treatment, meaning it’s used in addition to psychotherapy to improve its effectiveness. The focus on neuroplasticity and the potential for psychological breakthroughs during ketamine sessions are what truly set this modality apart. This approach seeks to create new neural pathways and disrupt entrenched addictive behaviors, offering a unique opportunity for healing and change.
Recovery and the Road Ahead: Long-Term Outlook
The goal of ketamine addiction therapy, like any addiction treatment, is sustained recovery and a higher quality of life. While ketamine can provide a powerful catalyst for change, the journey doesn’t end after the last session. Long-term recovery is a continuous process that requires ongoing commitment and support.
Post-treatment support is crucial. This often includes continued individual and group therapy, participation in support groups, and a focus on healthy lifestyle changes. Addressing the root causes of addiction, which often lie in untreated mental health conditions or past trauma, is vital for long-term success. Ketamine can help bring these issues to the surface, but consistent therapeutic work is needed to process and integrate these insights.
One of the most encouraging aspects of ketamine’s potential is its impact on long-term brain health. Chronic ketamine misuse can lead to cognitive impairments, but studies show that with sustained abstinence and proper treatment, cognitive function—including memory and attention span—can substantially improve within months to a year or more. The neuroplastic changes initiated by ketamine therapy may lay a foundation for this cognitive recovery, helping the brain “rewire” itself towards healthier patterns.
The potential for sustained abstinence is a key outcome. For example, studies have shown ketamine’s ability to prolong abstinence from alcohol and reduce cravings for cocaine. This doesn’t mean a magic bullet, but rather a powerful tool that, when used correctly, can significantly improve an individual’s chances of maintaining sobriety.
At Sober Steps, we believe in a holistic approach to recovery that extends far beyond initial treatment. We support individuals in building a foundation for lasting well-being. To learn more about our philosophy and comprehensive approach to recovery, visit our page on our comprehensive approach.
Current Research and Future Directions in Ketamine Treatment
The field of ketamine addiction therapy is still relatively young, but it’s rapidly expanding. Current research is focused on refining treatment protocols, understanding optimal dosages, and exploring its application across a wider range of substance use disorders.
We’ve seen promising results in pharmacological interventions for ketamine use disorder itself, with medications like naltrexone, lamotrigine, paliperidone palmitate, and bupropion showing potential for managing cravings and preventing relapse. Benzodiazepines and haloperidol have also demonstrated utility in managing acute ketamine intoxication and withdrawal.
Two clinical trials, one on cocaine addiction and another on alcohol dependency, have shown that people prescribed ketamine alongside therapy had better outcomes than those receiving therapy alone. A significant study on adjunctive ketamine for AUD demonstrated that ketamine infusions combined with relapse prevention-based psychological therapy led to a greater number of days abstinent from alcohol at six-month follow-up.
However, there are still significant gaps. A notable one is the gender disparity in research: in studies on ketamine use disorder treatment, only 27.7% of participants were female. Future research urgently needs to address this imbalance to ensure treatments are effective for all populations.
The need for larger, well-designed randomized controlled trials is paramount to confirm ketamine’s efficacy, establish optimal dosages, and understand its long-term safety profiles. Researchers are exploring different routes of administration, ideal frequencies, and how best to combine ketamine with various psychotherapies. We are committed to staying at the forefront of these developments, ensuring that the treatment options we connect individuals with are backed by the latest scientific evidence.
Frequently Asked Questions about Ketamine Treatment
Is ketamine addictive?
Yes, ketamine has the potential for psychological dependence, characterized by strong cravings and building a tolerance, though significant physical withdrawal symptoms are less common than with substances like opioids.
How is therapeutic ketamine different from street ketamine?
Therapeutic ketamine is administered in precise, controlled doses by medical professionals in a safe, monitored environment. Street ketamine is unregulated, its purity and dosage are unknown, and it is often mixed with other dangerous substances. The goal of therapeutic ketamine is healing and insight, while street ketamine is for recreational effects, often leading to misuse and harm.
Who is a good candidate for ketamine addiction therapy?
Candidates are typically individuals with a diagnosed substance use disorder, often co-occurring with conditions like treatment-resistant depression, who have not found success with traditional treatment methods. A thorough medical and psychological evaluation is required to ensure safety and suitability, as certain medical conditions (e.g., severe cardiovascular issues) may contraindicate ketamine treatment.
Conclusion
Ketamine, a substance with a complex history, is now emerging as a powerful tool in the fight against addiction. Its dual role as both a potential treatment and a substance of abuse underscores the critical importance of professional guidance and supervised care. We’ve explored how ketamine works in the brain, its promising therapeutic uses for depression and various addictions, and the significant risks associated with its misuse.
The promise of ketamine addiction therapy lies in its unique ability to promote neuroplasticity, open a “therapeutic window” for deeper psychological work, and potentially “rewire” the brain away from addictive patterns. This innovative approach, always integrated with comprehensive psychotherapy, offers new hope for individuals struggling with substance use disorders.
Addiction is a treatable condition, and recovery is always possible. At Sober Steps, we believe in empowering individuals with the knowledge and resources to make informed decisions about their treatment journey. If you or a loved one are seeking help, taking the first step towards a new life is the most courageous act of all.
To explore your options, please visit our page to find the right help for you.



